HQ Team
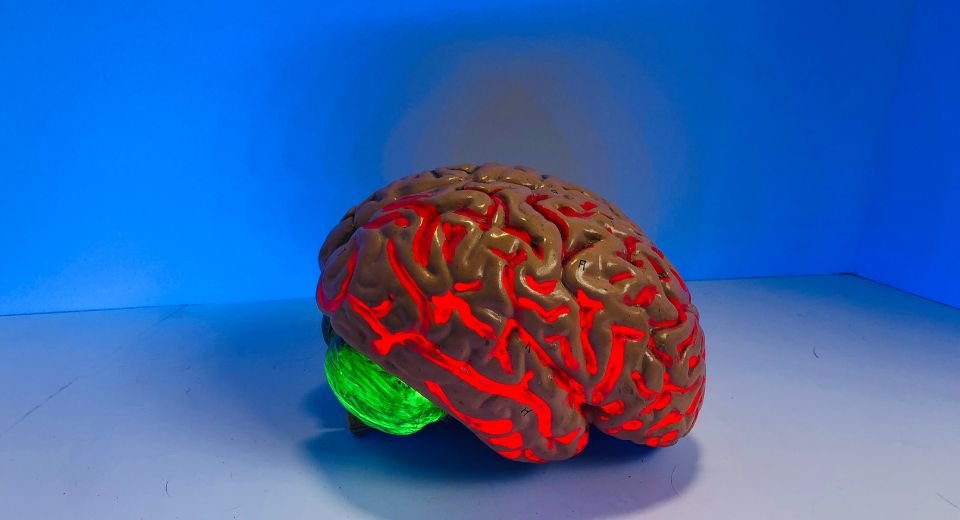
June 11, 2023: A blood protein, called fibrin, which supports clotting, is responsible for switching on detrimental genes in Alzheimer’s disease and multiple sclerosis, researchers say.
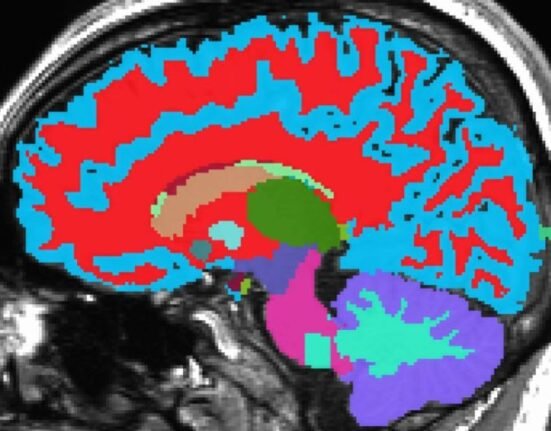
In both diseases immune cells known as microglia become harmful to neutrons, leading to cognitive dysfunction and motor impairment, researchers at Gladstone Institutes found.
These harmful immune cells may also contribute to age-related cognitive decline in people without dementia.
Microglia are brain cells that regulate the development, maintenance of neuronal networks, and repair injuries. They constantly patrol the cerebral microenvironment to respond to pathogens and damage.
Triggers
Scientists have been trying to understand the triggers responsible for turning good microglia bad, and their exact contribution to the disease.
If they could identify what makes microglia toxic, they could find new ways to treat neurological diseases.
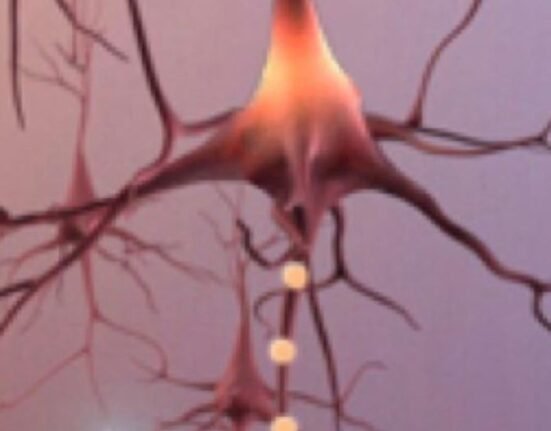
Led by senior investigator, Katerina Akassoglou, PhD, the study showed that harmful genes in microglia were turned on — destroying neurons — when blood leaked into the brain.
The scientists said fibrin was responsible for turning on the toxic genes in microglia.
“Our study answers, for the first time in a comprehensive way, how blood that leaks into the brain hijacks the brain’s immune system to cause toxic effects in brain diseases,” says Akassoglou, who is also director of the Center for Neurovascular Brain Immunology at Gladstone and a professor of neurology at UC San Francisco.
Effect of blood on brain
“Knowing how blood affects the brain could help us develop innovative treatments for neurological diseases.”
Individuals with neurological diseases have abnormalities in the brain’s network of blood vessels. This allows blood proteins to seep into brain areas responsible for cognitive and motor functions.
In the mice study, the researchers found that different blood proteins activate distinct molecular processes in microglia.
They identified that fibrin was responsible for driving unique gene and protein activities that make microglia toxic to neurons. The other blood proteins tested were not mainly responsible for these toxic effects.
Blood leaks in the brain occur early and correlate with worse prognosis in many of the diseases such as Alzheimer’s.
Latest tools
“We combined cutting-edge tools to capture a broad view of all the microglia processes triggered by distinct blood proteins,” said Andrew Mendiola, PhD, a scientist in Akassoglou’s lab and first author of the study.
“Fibrin stood out, as it triggered a dramatic gene response in microglia, which mirrored gene signatures identified in chronic neurological diseases such as Alzheimer’s disease.”
The researchers narrowed down fibrin’s negative influence to a specific inflammatory region of the protein.
This region does not impact fibrin’s critical role in blood clotting. In the study, the team showed that removing that inflammatory region reduced fibrin’s ability to turn on toxic genes in microglia, and restored the protective functions of these immune cells.
“We think that, across neurological diseases, fibrin deposits at sites of blood leaks might drive toxic immune responses,” Mendiola said. “Identifying approaches to selectively inhibit these toxic responses could be a game changer for treating disease.”
Human trials
Akassoglou’s lab has already developed one such drug, a therapeutic monoclonal antibody against fibrin’s inflammatory domain.
The antibody blocks the detrimental effects of fibrin without adverse effects on blood clotting and protects from multiple sclerosis and Alzheimer’s disease in mice.
A humanized version of this first-in-class fibrin immunotherapy has now started Phase 1 safety clinical trials.
The study was published in the journal Nature Immunology.
Gladstone Institutes is an independent, nonprofit life science research organization and is located in San Francisco.