HQ Team
October 3, 2023: The World Health Organization has recommended a second vaccine for the prevention of malaria in children to overcome a shortage of medicine, particularly in the African region.
The R21/Matrix-M vaccine, made by the Serum Institute of India, is expected to become available to countries in mid-2024 after two advisory groups of the global health agency suggested its use in children at risk of developing the disease.
The earlier RTS-S vaccine will be rolled out in some African countries at the beginning of 2024, according to a WHO statement.
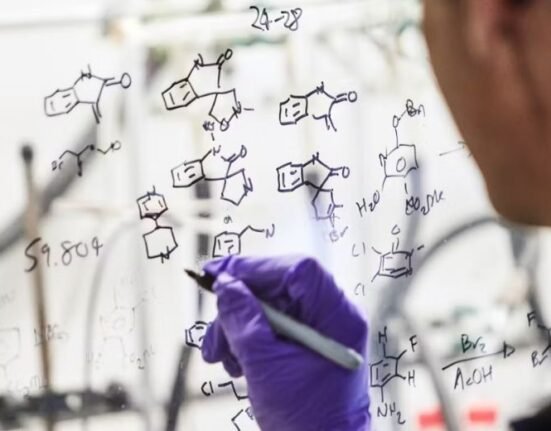
The vaccine was developed by the Jenner Institute at Oxford University and Serum Institute of India with support from the European and Developing Countries Clinical Trials Partnership, the Wellcome Trust, and the European Investment Bank.
To date, the R21 malaria vaccine has been licensed for use in Ghana, Nigeria and Burkina Faso.
‘Demand exceeds supply’
“As a malaria researcher, I used to dream of the day we would have a safe and effective vaccine against malaria. Now we have two,” said Dr Tedros Adhanom Ghebreyesus, WHO Director-General.
“Demand for the RTS-S vaccine far exceeds supply, so this second vaccine is a vital additional tool to protect more children faster and to bring us closer to our vision of a malaria-free future,” he said.
The recommendation follows advice from the WHO Strategic Advisory Group of Experts on Immunization (SAGE) and the Malaria Policy Advisory Group (MPAG) and was endorsed by the WHO Director-General following its regular biannual meeting held on 25-29 September.
Both vaccines were shown to be safe and effective in preventing malaria in children and, when implemented broadly, are expected to have a high public health impact.
Malaria, a mosquito-borne disease, majorly affects children in the African Region — where nearly half a million children die from the disease each year.
Demand for malaria vaccines is unprecedented. However, the available supply of RTS-S is limited. The addition of R21 to the list of WHO-recommended malaria vaccines is expected to result in sufficient vaccine supply to benefit all children living in areas where malaria is a public health risk, according to the statement.
Closing gap
“This second vaccine holds real potential to close the huge demand-and-supply gap,” said Dr Matshidiso Moeti, WHO Regional Director for Africa.
“Delivered to scale and rolled out widely, the two vaccines can help bolster malaria prevention and control efforts and save hundreds of thousands of young lives in Africa from this deadly disease.”
In areas with highly seasonal malaria transmission (where malaria transmission is largely limited to 4 or 5 months per year), the R21 vaccine was shown to reduce symptomatic cases of malaria by 75% during the 12 months following a three-dose series.
A fourth dose given a year after the third maintained efficacy. This high efficacy is similar to the efficacy demonstrated when RTS-S is given seasonally.
The vaccine showed a good efficacy of 66% during the 12 months following the first three doses. A fourth dose a year after the third maintained efficacy.
The vaccine has recently reached the primary one-year endpoint in a large-scale Phase III clinical trial – funded mainly by the Serum Institute of India, with Oxford University as the regulatory sponsor. The study parcipants included 4,800 children across Burkina Faso, Kenya, Mali and Tanzania. The Phase III trial results are under peer review before publication.
Lower costs
It is cost-effective at prices of $2 – $4 per dose and is comparable with other recommended malaria interventions and other childhood vaccines.
The two WHO-recommended vaccines, R21 and RTS-S, have not been tested in a head-to-head trial. “There is no evidence to date showing one vaccine performs better than the other. The choice of product to be used in a country should be based on programmatic characteristics, vaccine supply, and vaccine affordability.
The R21 vaccine was shown to be safe in clinical trials. “As with other new vaccines, safety monitoring will continue.”
At least 28 countries in Africa plan to introduce a WHO-recommended malaria vaccine as part of their national immunization programmes. Gavi, the Vaccine Alliance has approved providing technical and financial support to roll out malaria vaccines to 18 countries.
The Serum Institute of India has already established production capacity for 100 million doses per annum, which will be doubled over the next two years, according to a company statement.
The WHO’s recommendation is required for UNICEF to procure and GAVI to purchase the vaccine. The R21 malaria vaccine marked the culmination of 30 years of malaria vaccine research at the University of Oxford’s Jenner Institute.