HQ Team
April 20, 2024: A bacteria that causes infections, including pneumonia, bloodstream infections, and meningitis are being treated by doctors with less effective old generic antibiotics — even though the US regulator has cleared seven next-generation antibiotics to deal with the germs.
Researchers at the National Institutes of Health’s (NIH) Clinical Center found that the old antibiotics were also less safe in the treatment of diseases caused by gram-negative bacteria and cost was a major consideration while prescribing them.
Sameer Kadri, M.D., MS, Tenure Track Investigator in the National Institute of Health (NIH) Clinical Center’s Critical Care Medicine Department at NIH Clinical Center, said clinicians in US hospitals still treated more than 40% of patients battling highly resistant pathogens exclusively with older, generic agents, even when these older agents are already known to be highly toxic or sub-optimally effective.
Gram-negative bacteria are resistant to multiple drugs and are increasingly resistant to most available antibiotics. These bacteria have built-in abilities to find new ways to be resistant and can pass along genetic materials that allow other bacteria to become drug-resistant as well, according to Centers for Disease Control and Prevention.
Decision-making process
The NIH researchers examined the factors influencing doctors’ preference for newer antibiotics over traditional generic agents to shed light on the decision-making processes among clinicians when treating patients with challenging bloodstream infections caused by gram-negative bacteria and significant comorbidities.
They found that in a considerable proportion of hospitals, particularly smaller facilities located in rural areas, staff were reluctant to adopt newer antibiotics.
“Researchers identified a large cost disparity between older and newer classes of antibiotics; the newer drugs can cost approximately six times more than the older medications, which could disincentivize prescribing,” according to an NIH statement.
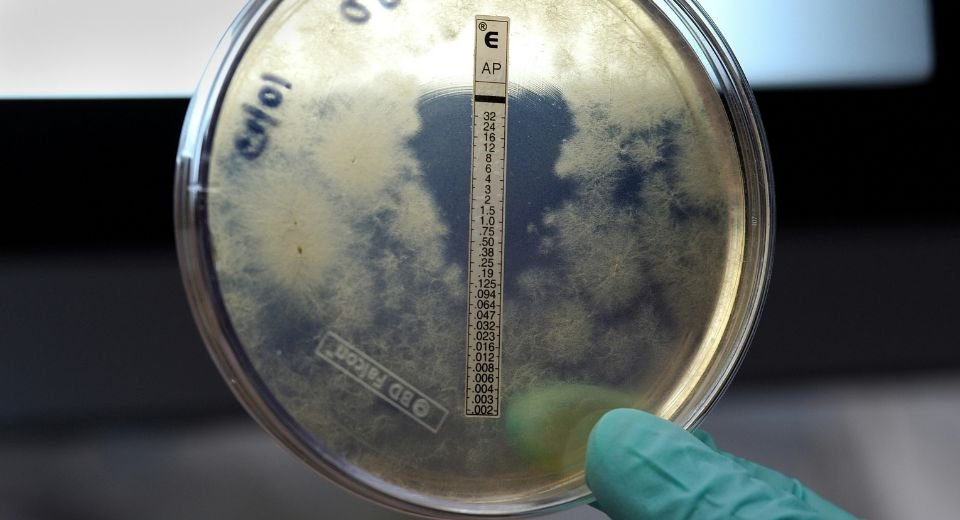
Laboratory results
The US Food and Drug Administration has recently approved gram-negative antibiotics (ceftazidime–avibactam, ceftolozane–tazobactam, meropenem–vaborbactam, plazomicin, eravacycline, imipenem–relebactam–cilastatin, and cefiderocol) between 2014 and 2019.
Between the first quarter of 2016 and second quarter of 2021, ceftolozane–tazobactam (approved 2014) and ceftazidime–avibactam (2015) predominated new antibiotic usage whereas subsequently approved gram-negative antibiotics saw relatively sluggish uptake, according to the researchers.
The study was conducted in adult inpatients in 619 US hospitals.
Researchers stated that next-gen agents were prescribed more often at hospitals where lab results that showed the medications were effective against a patient’s bacterial infection “are reported to prescribers.”
Scientists suggest that earlier and more widespread availability of such lab testing might improve use.
“This sluggish uptake is an important issue because it threatens future development and supply of new antibiotics for patients,” Dr. Kadri said.