HQ Team
June 4, 2024: Researchers at the National Institutes of Health have developed an artificial intelligence tool that uses a simple blood test to predict if cancer responds to immunotherapy drugs.
The tool uses routine clinical data to forecast if the immune cells are capable of killing cancer cells and the machine-learning model may help doctors determine if immunotherapy drugs are effective for treating a patient’s cancer.
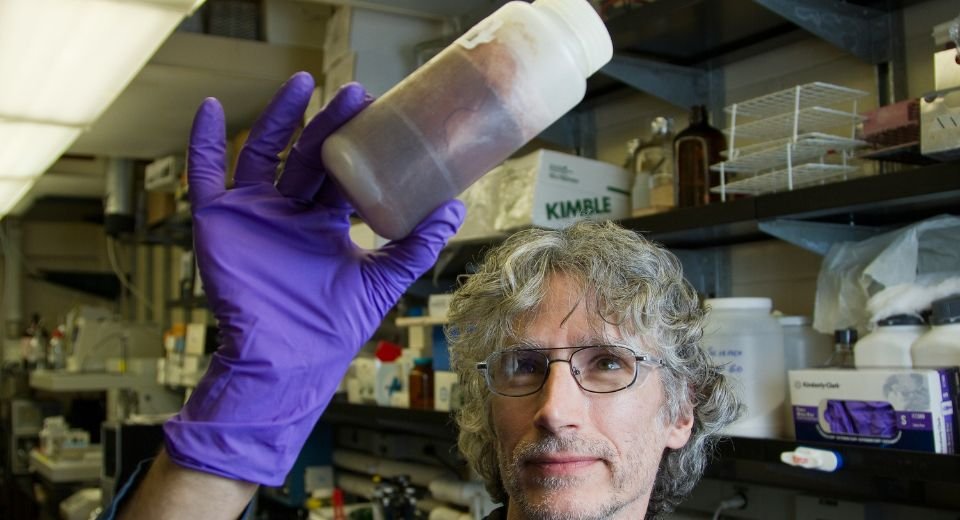
A proof-of-concept study was led by researchers at the National Cancer Institute’s (NCI) Center for Cancer Research and Memorial Sloan Kettering Cancer Center in New York.
Presently, two predictive biomarkers have been approved by the Food and Drug Administration for use in identifying patients who may be candidates for treatment with immune checkpoint inhibitors.
Mutational burden
The first is tumour mutational burden, which is the number of mutations in the DNA of cancer cells. The second is PD-L1, a tumour cell protein that limits the immune response and is a target of some immune checkpoint inhibitors.
These biomarkers do not always accurately predict response to immune checkpoint inhibitors. Recent machine-leaning models that use molecular sequencing data have shown value in predicting response, but this kind of data is expensive to obtain and not routinely collected.
The National Institutes of Health study made a different kind of machine-learning model that makes predictions based on five clinical features that are routinely collected from patients.
2,881 patients
It includes a patient’s age, cancer type, history of systemic therapy, blood albumin level, and blood neutrophil-to-lymphocyte ratio, a marker of inflammation. The model also considers tumour mutational burden, assessed through sequencing panels.
The model called the Logistic Regression-Based Immunotherapy-Response Score, was constructed and evaluated using data from multiple independent data sets that included 2,881 patients treated with immune checkpoint inhibitors across 18 solid tumour types.
It accurately predicted a patient’s likelihood of responding to an immune checkpoint inhibitor and how long they would live, both overall and before the disease returned.
It was also able to identify patients with low tumour mutational burden who could still be treated effectively with immunotherapy., according to the researchers.
The National Institutes of Health is the primary agency of the United States government responsible for biomedical and public health research.