HQ Team
August 7, 2024: Scientists at Northwestern University’s Simpson Querrey Institute for BioNanotechnology have invented a bioactive material to successfully regenerate cartilage in the knee joints of sheep.
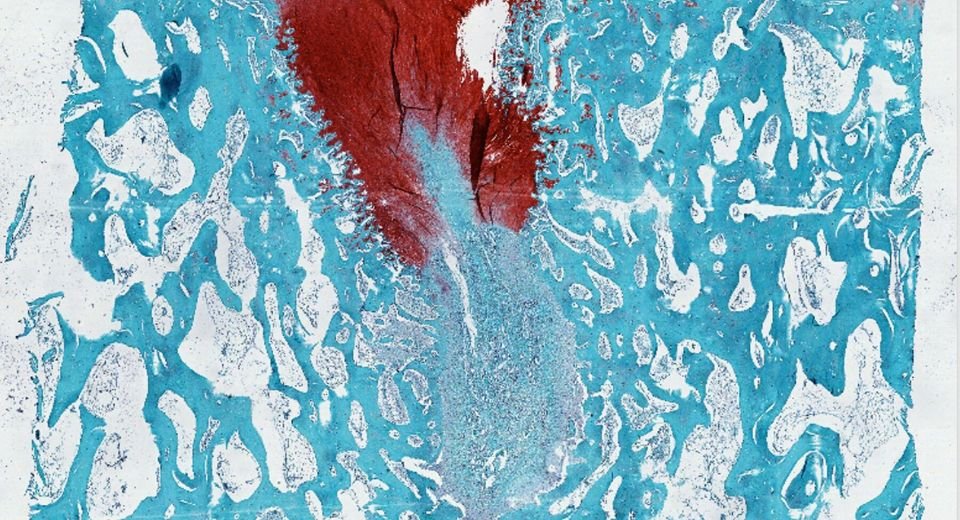
The material which looks like rubbery goo, comprises peptides, proteins and polysaccharides that mimic the microstructure of natural cartilage, and within six months, researchers observed new cartilage growth, according to a statement.
Much like humans, sheep cartilage is stubborn and incredibly difficult to regenerate. Sheep stifles and human knees also have similarities in weight bearing, size and mechanical loads.
“A study on a sheep model is more predictive of how the treatment will work in humans,” said Northwestern’s Samuel I. Stupp, who led the study. “In other smaller animals, cartilage regeneration occurs much more readily.”
Rubbery matrix
Researchers injected the thick, paste-like material into cartilage defects, where it transformed into a rubbery matrix. Not only did new cartilage grow to fill the defect as the scaffold degraded, but the repaired tissue was consistently higher quality compared to the control group, according to the statement.
The researchers said the new material “someday could potentially be used to prevent full knee replacement surgeries, treat degenerative diseases like osteoarthritis and repair sports-related injuries like ACL tears” or anterior cruciate ligament tears.
“When cartilage becomes damaged or breaks down over time, it can have a great impact on people’s overall health and mobility,” Stupp said.
“The problem is that, in adult humans, cartilage does not have an inherent ability to heal. Our new therapy can induce repair in a tissue that does not naturally regenerate. We think our treatment could help address a serious, unmet clinical need.”
Hyaluronic acid
The new biomaterial comprises two components.
One is a bioactive peptide that binds to transforming growth factor beta-1 (TGFb-1) — an essential protein for cartilage growth and maintenance — and modified hyaluronic acid, a natural polysaccharide present in cartilage and the lubricating synovial fluid in joints.
“Many people are familiar with hyaluronic acid because it’s a popular ingredient in skincare products,” Stupp said.
“It’s also naturally found in many tissues throughout the human body, including the joints and brain. We chose it because it resembles the natural polymers found in cartilage.”
Within just six months, the researchers observed evidence of enhanced repair, including the growth of new cartilage containing the natural biopolymers (collagen II and proteoglycans), which enable pain-free mechanical resilience in joints.
Fibrocartilage vs hyaline cartilage
The current standard of care for degenerative diseases is microfracture surgery, during which surgeons create tiny fractures in the underlying bone to induce new cartilage growth.
“The main issue with the microfracture approach is that it often results in the formation of fibrocartilage — the same cartilage in our ears — as opposed to hyaline cartilage, which is the one we need to have functional joints,” Stupp said.
“By regenerating hyaline cartilage, our approach should be more resistant to wear and tear, fixing the problem of poor mobility and joint pain for the long term while also avoiding the need for joint reconstruction with large pieces of hardware.”
The study will be published in the Proceedings of the National Academy of Sciences.