HQ Team
May 20, 2024: The World Health Organization, after seven years, has updated its pathogens list which has 15 families of antibiotic-resistant bacteria grouped into critical, high and medium categories for prioritisation.
The latest list saw the removal of five pathogen-antibiotic combinations that were included in 2017, and the addition of four new combinations.
The critical priority pathogens list includes gram-negative bacteria resistant to last-resort antibiotics, and Mycobacterium tuberculosis resistant to the antibiotic rifampicin, which present major global threats due to their high burden, and ability to resist treatment and spread resistance to other bacteria, according to a WHO statement.
Gram-negative bacteria have built-in abilities to find new ways to resist treatment and can pass along genetic material that allows other bacteria to become drug-resistant as well.
The gram-negative bacteria can cause disease in humans and can reach almost all systems in the organism, such as the digestive system, nervous system, urinary system, and bloodstream, causing diarrheal gastroenteritis until severe meningitis.
Immunocompromised
Such microorganisms colonise the intestines, airways, and skin, which favours the spread to other parts of the human organism, especially in immunocompromised individuals.
Gastroenteritis caused by enterobacteriaceae (Shigella sapp., Salmonella sapp., enteropathogenic E. Coli, affects millions of people worldwide and is related to a lack of sanitation.
They are responsible for meningitis — a potentially fatal disease if not treated in time — and it is acquired both in the community and the hospital environment. Urinary tract infections are also common, especially in young women.
These infections became a problem with the rampant emergence of multi-resistant bacteria. Bacteremia is an important complication of these infections.
“By mapping the global burden of drug-resistant bacteria and assessing their impact on public health, this list is key to guiding investment and grappling with the antibiotics pipeline and access crisis,” said Dr Yukiko Nakatani, WHO’s Assistant Director-General for Antimicrobial Resistance ad interim.
AMR intensifies
“Since the first Bacterial Priority Pathogens List was released in 2017, the threat of antimicrobial resistance has intensified, eroding the efficacy of numerous antibiotics and putting many of the gains of modern medicine at risk.”
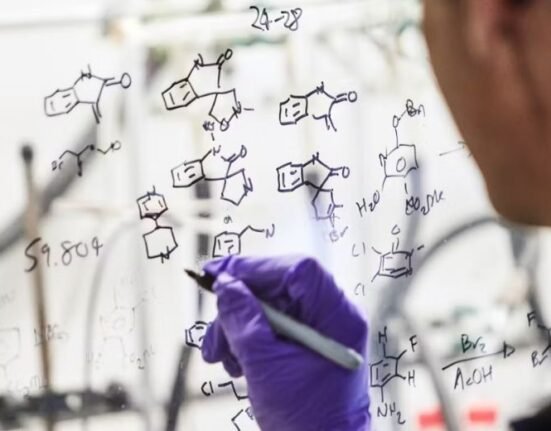
The list provides guidance on the development of new and necessary treatments to stop the spread of antimicrobial resistance.
Antimicrobial resistance (AMR) occurs when bacteria, viruses, fungi, and parasites no longer respond to medicines, making people sicker and increasing the risk of disease spread, illness and death.
AMR is driven in large part by the misuse and overuse of antimicrobials. The updated list incorporates new evidence and expert insights to guide research and development for new antibiotics and promote international coordination to foster innovation.
The WHO has placed salmonella and shigella on the high-priority pathogen list. They cause a high burden in low- and middle-income countries, along with Pseudomonas aeruginosa and Staphylococcus aureus, which pose significant challenges in healthcare settings.
Tuberculosis
Other high-priority pathogens, including antibiotic-resistant Neisseria gonorrhoeae and Enterococcus faecium, present unique public health challenges, including persistent infections and resistance to multiple antibiotics, necessitating targeted research and public health interventions, according to the WHO.
Medium-priority pathogens include two new entrants in the list — Group A and B Streptococci and others such Streptococcus pneumoniae, and Haemophilus influenzae. These pathogens require increased attention, especially in vulnerable populations including paediatric and elderly populations, particularly in resource-limited settings.
“Antimicrobial resistance jeopardises our ability to effectively treat high-burden infections, such as tuberculosis, leading to severe illness and increased mortality rates,” said Dr Jérôme Salomon, WHO’s Assistant Director-General for Universal Health Coverage, Communicable and Noncommunicable Diseases.
The global health agency also approved the designation of 33 national and regional regulatory authorities as WHO Listed Authorities (WLAs) that can be relied on for fulfilling the highest level of regulatory standards and practices for the quality, safety and efficacy of medicines and vaccines.
This listing makes a total of 36 regulatory authorities from 34 Member States now designated as WLAs since the start of the initiative in March 2022, according to a separate statement.