HQ Team
July 22, 2023: Urinary tract infections (UTIs) affect nearly one in two women at least once in their lifetime. The growing concern about antibiotic resistance in UTIs has become a significant challenge for physicians worldwide. More than 92 percent of bacteria that cause UTIs are resistant to at least one common antibiotic, and almost 80 percent are resistant to at least two, according to a 2019 study.
Researchers from ETH Zurich, in collaboration with Balgrist University Hospital, have developed a rapid test that utilizes genetically modified bacteriophages to tackle these infections effectively.
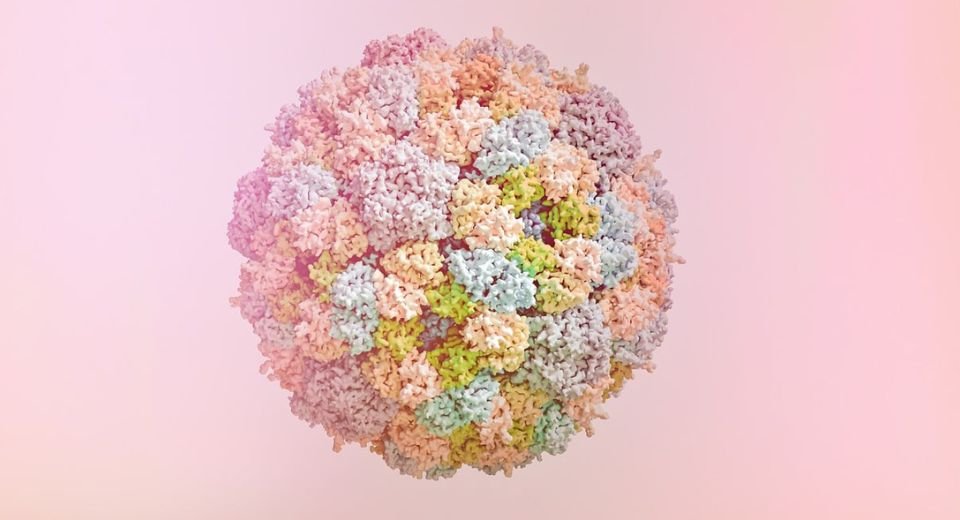
The team at ETH Zurich’s food microbiology research group, led by Professor Martin Loessner, explored the potential of bacteriophages, which are highly specialized viruses that infect specific types or strains of bacteria. The researchers identified phages effective against the three main culprits of UTIs: Escherichia coli, Klebsiella, and Enterococci. These natural phages were then genetically modified to produce an easily detectable light signal when they infect their target bacteria.
Speedy results
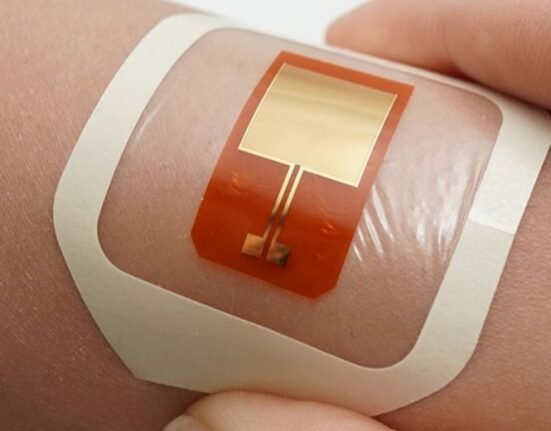
More importantly, these tests give speedy results. In less than four hours, the researchers were able to reliably detect pathogenic bacteria directly from a urine sample. This breakthrough paves the way for faster and more accurate diagnoses, allowing physicians to prescribe suitable antibiotics immediately after confirmation, thereby minimizing the development of antibiotic resistance and improving antibiotic stewardship.
Moreover, the rapid test also holds the potential to predict patients who would respond particularly well to tailored phage therapy. The strength of the light signal produced during the assay indicates the phages’ efficiency in attacking the bacterium. Consequently, the brighter the sample glows, the better the bacterium’s response to the therapy, offering a personalized treatment approach.
Phage action
Phages are now experiencing a comeback due to rampant antibiotic resistance. Phages are not new and have been in use for a century, but they were relegated to the background after the discovery of penicillin. The advantage of phage therapy lies in its specificity, targeting only the specific bacterial strain responsible for the infection.
“Phages aren’t interested in completely killing their host, the pathogenic bacterium,” explains researcher Samuel Kilcher, one of the study’s two final authors.
To further enhance the efficacy of phages, the researchers genetically modified them to produce not only new phages inside the infected host bacterium but also bacteriocins – potent bacteria-killing proteins. This dual attack strategy proves especially effective against bacterial strains that have altered their surface to evade phage recognition, making the treatment more potent.
Worldwide, numerous academic and commercial clinical trials are actively exploring the potential of natural and genetically optimized phages in combating antibiotic resistance.
Researchers say that there is still a long way to go before phage therapies become widely applicable. Extensive clinical studies and regulatory adjustments are required, considering that phages are biological entities that co-evolve with their bacterial hosts.
As a proof of concept, the researchers now plan to test the efficacy of the new phage therapy in a clinical trial involving selected patients. If successful, this innovative approach could revolutionize the management of recurrent cystitis and other urinary tract infections, offering hope for a future where antibiotic resistance is better controlled, and patient outcomes significantly improved.
Another Canadian study, led by Dr. Greg German, an infectious disease physician at St. Joseph’s Hospital, is using phages for treatment-resistant UTIs.
The study is available here.