HQ Team
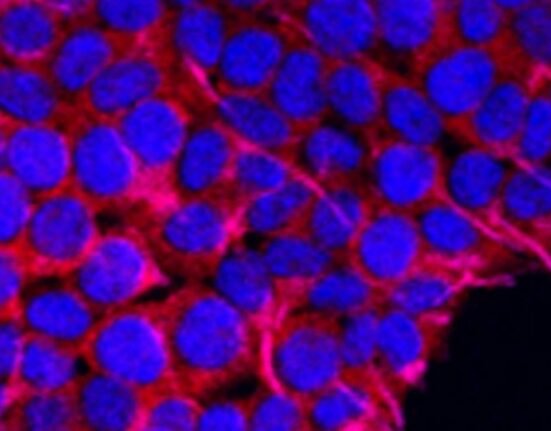
February 18, 2023: Activation of bio-therapeutic drugs by switching to LEDs embedded close to a tumor may be cancer immunotherapy’s future, researchers found.
Cancer treatments like chemotherapy kill cancer cells, but they can also damage healthy cells in your body, such as blood and skin cells.
“This means that they can cause side effects, including hair loss, feeling tired and sick, and they also put patients at increased risk of picking up infections,” said Dr Amit Sachdeva from the Norwich, UK-based University of East Anglia’s School of Chemistry.
“There has therefore been a huge drive to create new treatments that are more targeted and don’t have these unwanted side effects,” he said in a statement on the university’s website.
“Several antibodies and antibody fragments have already been developed to treat cancer. These antibodies are much more selective than the cytotoxic drugs used in chemotherapy. However, they can still cause severe side effects, as antibody targets are also present in healthy cells,” Dr Schdeva said.
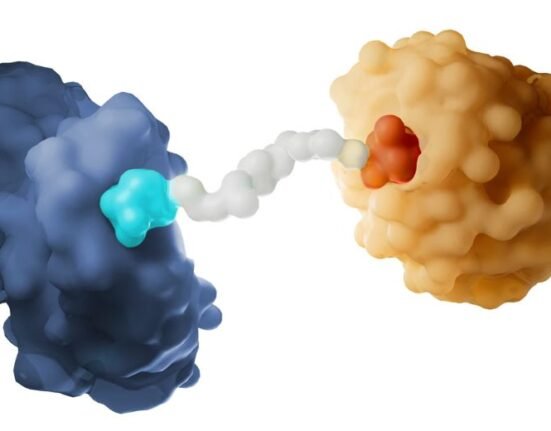
Covalent bond
The university’s team engineered one of the first antibody fragments that bind to and forms a covalent bond with its target — upon irradiation with UV light of a specific wavelength.
A covalent bond relates to or denotes chemical bonds formed by sharing electrons between atoms.
“A covalent bond is like melting two pieces of plastic and fusing them. It means that drug molecules could, for example, be permanently fixed to a tumour,” Sachdeva said.
It means that immunotherapy treatments could be engineered to attack tumours more precisely than ever before. The team has engineered antibody fragments that not only fuse with their target but are also light-activated.
The team hopes their work will lead to the development of highly targeted light-responsive bio-therapeutics.
Dr Sachdeva said: “This would mean that antibodies could be activated at the tumour site and covalently stick to their target upon light activation.
Treatment highly-targeted
“In other words, you could activate antibodies to attack tumour cells by shining light – either directly onto the skin, in the case of skin cancer, or using small LED lights that could be implanted at the site of a tumour inside the body.”
The treatment would be highly targeted and more effective than current state-of-the-art cancer immunotherapies.
“This would make cancer treatment more efficient and targeted because it means that only molecules in the vicinity of the tumour would be activated, and it wouldn’t affect other cells. Dr Sachdeva said this could reduce patient side effects and improve antibody residence time in the body.
“It would work for skin cancer, or where there is a solid tumour – but not for blood cancers like leukaemia.”
If successful in the following stages of their work, the researchers hope to see the ‘next generation’ light-activated immunotherapies being used to treat cancer patients within five to 10 years.