HQ Team
August 6, 2024: Contineum Therapeutics, Inc., a US San Diego-headquartered biopharmaceutical company’s trial drug may reverse multiple sclerosis damage by potentially restoring movement and function.
The trial showed “encouraging preclinical data” on an experimental drug, dubbed PIPE-307, in patients with relapse-remitting multiple sclerosis, according to a company statement.
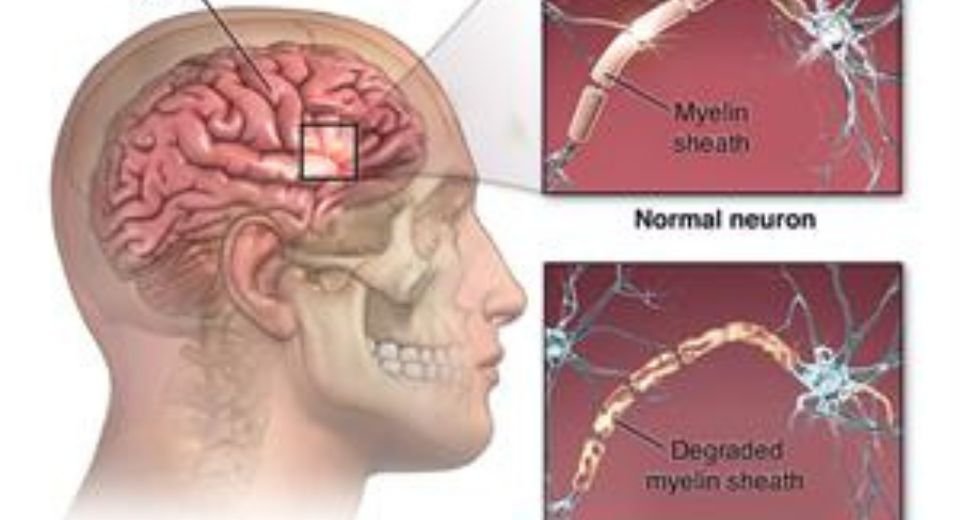
Multiple sclerosis is a disease of the brain and immune system. The brain contains a network of billions of neurons, nerve cells that send messages telling mouth to speak, legs to move and lungs to breathe.
Each neuron is wrapped in myelin, a protective coating like the plastic sheath around a copper electrical wire.
With multiple sclerosis, our immune system – which normally protects against germs – mistakes myelin for a foreign invader. This case of mistaken identity prompts an all-out assault.
Frayed power cords
The immune system attacks the myelin, short-circuiting our neurons like frayed power cords.
“Over time, the connections between nerves are lost, and nerve cells die. Multiple sclerosis robs people of basic functions we take for granted – vision, sensation, motor strength … and sometimes …even the ability to speak, eat or breathe independently,” University of California San Francisco Neurology Professor Stephen Hauser, MD, said.
Contineum’s laboratory drug is being developed with the help of scientists at the University of California San Francisco. It is being tested under a global license and development agreement between Contineum and Janssen Pharmaceutica NV.
Contineum has two drug candidates in clinical trials. One is PIPE-791 for idiopathic pulmonary fibrosis and progressive multiple sclerosis. Its PIPE-307 is the second for relapse-remitting multiple sclerosis.
Johnson and Johnson, the parent company of Janssen Pharmaceuticals, has started mid-stage trials of the second test drug this year.
Efficacy, safety
The mid-stage trial, named VISTA, will assess efficacy and safety in patients with relapse-remitting multiple sclerosis and is designed to measure multiple clinical and imaging endpoints sensitive to changes in remyelination in the disease, according to the statement.
For decades, doctors suspected that T-cells – a type of white blood cell that acts like the immune system’s detectives to identify intruders – were behind the myelin attacks.
By the 1980s, Hauser had developed a means to test this theory, after gathering evidence that another immune soldier, B-cells, were the real culprits.
Human bodies are built to protect our brains and nervous system from infections, keeping them safe behind what doctors call the “blood-brain barrier” – a cellular city wall.
Professor Hauser proved that in multiple sclerosis, T-cells disrupted this barrier, opening the proverbial city gates, but it was B-cells and the proteins they produce that attacked nerve cells’ myelin coatings, short-circuiting the brain’s network of neurons.
Ofatumumab
Rituximab, which killed B-cells, had been too risky for federal funding but not for industry.
Pharmaceutical company Genentech, co-founded by UCSF professors, agreed to fund what would become a successful trial of the drug as a treatment for the disease.
Rituximab stopped the disease virtually in its tracks, changing the face of MS forever.
The breakthrough led to the 2017 development of a second medicine, ocrelizumab and then a third, ofatumumab, in 2020, also pioneered by Hauser and his UCSF colleagues working closely with industry partners.
Slower signal tranmission
Relapse-remitting multiple sclerosis is the most common form of multiple sclerosis. The pathological hallmark of all forms of multiple sclerosis is the accumulation of demyelinating lesions that occur in the brain and spinal cord.
In healthy neurons, myelin, which is a specialized extension of the plasma membrane of oligodendrocytes, serves as an insulator that allows for rapid and efficient conduction of electrochemical signals along the axon.
In demyelinating diseases, such as multiple sclerosis, loss of myelin leads to slower signal transmission through the axon and eventual permanent loss of neuronal function.