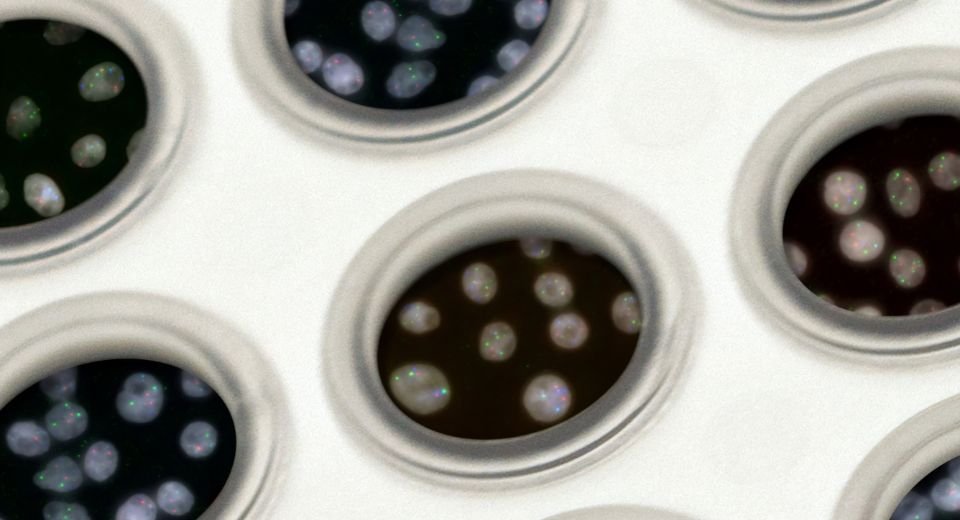
Cancer genome; NCI picture
HQ Team
October 3, 2022: Regular screening and checkups for cancer can help improve outcomes as they can be detected early before they have a chance to spread.
Screenings for cancer among people at risk have helped halve cervical deaths and prevented 12,000 breast cancer deaths in the U.S. annually. Almost all women diagnosed with breast cancer at the earliest stage survive for at least 5 years. And survival rates for stage 1 lung cancer could exceed 90%, according to a landmark study published in the New England Journal of Medicine. More than 9 in 10 bowel cancer patients in England survive the disease for 5 years or more if diagnosed at the earliest stage.
Cancers without available screenings account for 70% of cancer deaths among those aged 50 to 79 years.
Early detection tests Current MCED Scenario
Some annual screenings require just a blood test for people at risk. Multi-cancer early detection (MCED) tests can reveal cancers with a single blood draw. These tests measure biological signals or biomarkers in body fluids (liquid biopsies)that may be shed by cancer cells. The screening can test for several cancers depending on which biomarker one is looking for.
Here’s why these tests could be valuable enough to become part of your annual physical.
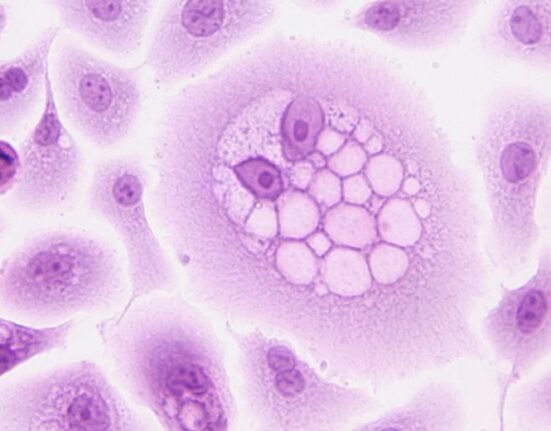
Until recently, only a few biomarkers could be recognized for cancer, but technology has enabled scientists to identify and analyze even the smallest genetic fragments for cancer.
Testing for cancer can be a lengthy and invasive procedure. MCED blood tests are simpler, affordable, convenient, and not harmful. The World Economic Forum has identified liquid biopsy as one of the world’s top 10 emerging technologies
Preventive screening is currently recommended for five types of cancer: breast, colorectal, cervical, prostate, and lung (for high-risk individuals).
“There’s a laundry list of things in the blood that can tell you about the presence of cancer,” says Samir Hanash, M.D., Ph.D., a member of the National Cancer Institute’s Early Detection Research Network. “These include circulating DNA (ctDNA), RNA, and proteins being shed by tumours.” Prostate-specific antigen (PSA) levels, for one, are known to rise in response to malignant cells in the gland, while patients with ovarian cancer commonly have elevated levels of cancer antigen 125 (CA125), he adds.
MCED tests are different from genetic screening markers as they measure current cancer marker levels. “They’re meant to catch cancer when it’s still kind of small,” Dr Hanash says. “You’re looking for the presence of cancer, but you don’t want to wait until a disease has spread to the brain or organs when it’s not usually treatable.”
“With blood biomarkers, there are trajectory-based calculations that could help define if somebody is likely to have cancer growing in their body or not,” explains Dr Hanash. A value that goes from low to high is a red flag. “You’re not waiting to see if it reaches a high…value before determining someone has cancer.”
Current MCED scenario
New MCED tests in development can detect a common cancer signal from over 50 different types of cancer and predict where the signal has come from in the body.
At the recently held European Society for Medical Oncology or ESMO Congress 2022, a PATHFINDER study reported that an MCED test detected a cancer signal in 1.4% of 6621 people aged 50 years and over who were not known to have cancer, and cancer was confirmed in 38% of those with a positive test. Of 6290 cancer-free people, 99.1% received a negative test result. Among those with positive test results, the time to achieve diagnostic resolution was an average 79 days. Among participants with a positive screening test, a diagnostic resolution was achieved within three months for 73%.
MCED tests have been available in China, Japan, and South Korea for decades. In Europe and the U.S. they are still not common and are costly.
For around $200 a test, at least one American company, 20/20 GeneSystems, Inc. (20/20), offers an MCED test called OneTest™ for Cancer. It combines the results of six protein (tumour antigen) biomarkers, including the antigens associated with cancers of the lungs, liver, pancreas, ovaries and intestines, among others.
MCED tests that can detect signals from a wide range of cancers using next-generation genomic sequencing (NGS) technology are: CancerSEEK from Thrive, Galleri from GRAIL, GENECAST’s ADPSTM, PanSeer from SINGLERA Genomics and PREDICT from Burning Rock.
Clinical validation of the overall clinical practice has yet to be evaluated for the above-mentioned tests.
Governments and public health institutes are actively investing in MCED research, with the National Cancer Institute in the U.S. receiving $75 million for a pilot study.
A note of caution here is necessary. These MCED liquid biopsies are not definitive diagnoses. Any detections need to be followed up with further tests such as imaging to confirm the diagnosis, determine tumour presence and stage, and identify its exact location.
Such screenings may soon become a part of health checkups. “You get your blood checked for cholesterol,” points out Dr Hanash. “If there’s a nice-performing test out there, why not have another tube of blood taken to test for cancer?”