HQ Team
April 3, 2024: Humans’ lack of immunity may rapidly result in the transmission of bird flu among people if the avian influenza virus acquires the ability to spread quickly, according to the European Food Safety Authority (EFSA).
The EU body’s warning comes after the Texas Department of State Health Services reported on April 1, a human case of avian influenza A(H5N1) virus in Texas, US.
The case was identified as a person who had direct exposure to dairy cattle presumed to be infected with avian influenza. The patient had experienced eye inflammation as their only symptom.
The patient had a confirmatory test conducted by the Centers for Disease Control and Prevention over the weekend, according to a TDSHS statement.
“The patient is being treated with the antiviral drug oseltamivir. The case does not change the risk for the general public, which remains low.”
Second case
According to the CDC, this is the second human case of H5N1 flu in the US and the first linked to exposure to cattle.
“If avian A(H5N1) influenza viruses acquire the ability to spread efficiently among humans, large‐scale transmission could occur due to the lack of immune defences against H5 viruses in humans,” according to the EFSA’s scientific report.
The authority is an EU body that provides independent scientific advice and communicates on existing and emerging risks associated with the food chain.
Avian influenza viruses remained prevalent among wild bird populations in the European Union and European Economic Area, leading to significant illness and death of birds, the EFSA stated.
Fur animal farms
Transmission between bird and mammal species has been observed, particularly in fur animal farms, where outbreaks have been reported.
“While transmission from infected birds to humans is rare, there have been instances of exposure to these viruses since 2020 without any symptomatic infections reported in the EU and the European Economic Area.”
As these viruses continue to evolve globally, and with the migration of wild birds, new strains carrying potential mutations for mammalian adaptation could be a result.
Cats living in households and with access to the outdoors could also be a potential vehicle for transmission.
Other than poultry and dairy cows reported in the US, mammals hit by the virus include goats, cats, foxes, racoons, skunks, polar and grizzly bears and elephant seals.
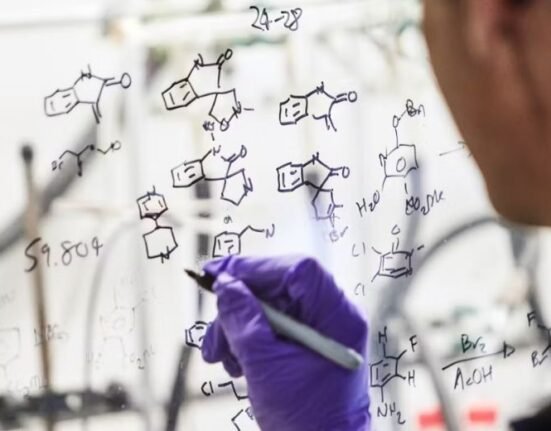
Intrinsic and extrinsic drivers
The new forms of the viruses capable of infecting mammals, including humans, can be facilitated through “intrinsic drivers are related to virus characteristics or host susceptibility.”
Extrinsic drivers may increase the exposure of mammals and humans to AIV thereby stimulating mutation and adaptation to mammals.
Extrinsic drivers include the ecology of host species, such as including wildlife, human activities like farming practices and the use of natural resources, and climatic and environmental factors.
The EFSA called for actions including enhancing surveillance targeting humans and animals, ensuring access to rapid diagnostics, promoting collaboration between animal and human sectors, and implementing preventive measures such as vaccination.
Biosecurity measures
It urged for strengthening veterinary infrastructure, enforcing biosecurity measures at farms, and reducing wildlife contact with domestic animals.
From January 1, 2003, to February 26, 2024, a total of 254 cases of human infection with avian influenza A(H5N1) virus have been reported from four countries within the Western Pacific Region., according to the WHO.
Of these cases, 141 were fatal, resulting in a case fatality rate (CFR) of 56%. The last cases in the Western Pacific Region were reported from Vietnam, with an onset date of March 11, 2024.
Globally, from January 1, 2003, to February 26, 2024, about 887 cases of human infection with the virus were reported from 23 countries.
Of these 887 cases, 462 were fatal, with a case fatality rate of 52%.