HQ Team
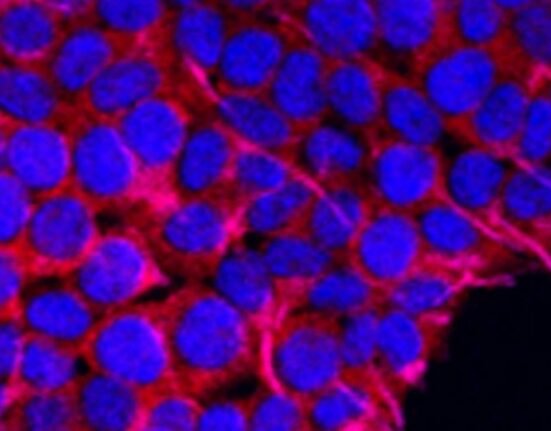
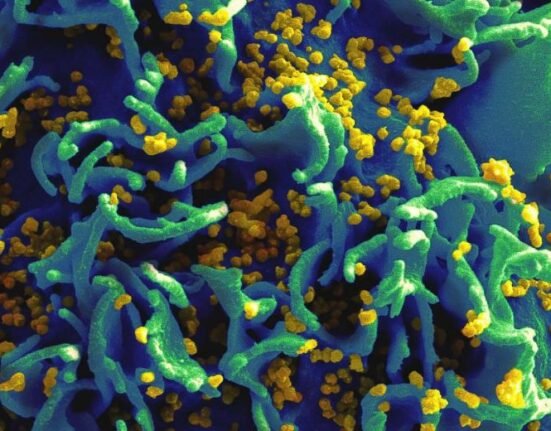
March 12, 2025: In a significant development for HIV prevention, Gilead Sciences has unveiled promising data from its Phase 1 study evaluating two novel, once-yearly formulations of lenacapavir, the company’s long-acting injectable HIV-1 capsid inhibitor. Gilead plans to advance the drug into a Phase 3 study in the second half of 2025, marking a critical step toward offering a once-yearly HIV prevention solution.
The findings were presented at the Conference on Retroviruses and Opportunistic Infections (CROI 2025) and published in The Lancet.
Phase 1 trial: Efficacy and safety
The Phase 1 study assessed the pharmacokinetics, safety, and tolerability of two intramuscular formulations of lenacapavir, each administered as a single 5,000 mg dose. The trial involved 40 healthy adults aged 18 to 55, with a body mass index (BMI) of ≤35.0 kg/m², who were at low risk of HIV acquisition. The results were highly encouraging.
Both formulations maintained plasma concentrations above the 95% effective threshold for at least 56 weeks. At Week 52, median trough concentrations for the two formulations (57.0 ng/mL and 65.6 ng/mL) exceeded those observed with the twice-yearly lenacapavir formulation in the trials (23.4 ng/mL at Week 26).
Both formulations were well-tolerated, with no new safety signals. The most common adverse event was mild injection site pain, which resolved within a week for most participants.
These findings suggest that once-yearly lenacapavir could provide a highly effective and convenient PrEP option, addressing adherence challenges associated with daily or even twice-yearly regimens.
The Phase 1 data build on the success of Gilead’s PURPOSE 1 and PURPOSE 2 trials, which evaluated twice-yearly subcutaneous lenacapavir for PrEP. These trials demonstrated that lenacapavir was superior to both background HIV incidence rates and once-daily oral Truvada (F/TDF) in reducing HIV infections across diverse populations. The new once-yearly formulations aim to further simplify HIV prevention by reducing the frequency of dosing to just once per year.
In a survey of 2,561 cisgender women in sub-Saharan Africa, approximately two-thirds preferred twice-yearly lenacapavir injections over once-daily pills.
61% of respondents felt more protected from HIV with twice-yearly injections. 61% reported greater confidence in not missing a dose with the long-acting option. Adolescents, in particular, noted that twice-yearly injections better suited their lifestyles compared to daily pills.
The PURPOSE 1 trial also broke new ground by intentionally including adolescents aged 16 and 17, a population often underrepresented in clinical trials. Of the 124 adolescents enrolled, 56 were assigned to the lenacapavir group. The data showed comparable pharmacokinetic and safety profiles between adolescents and adults, with no incident HIV infections in either group. These results support the potential use of lenacapavir for adolescents who need or want PrEP, pending regulatory approval.
Next steps: Phase 3 study
Gilead’s decision to advance once-yearly lenacapavir directly to Phase 3 trials underscores the drug’s potential to transform HIV prevention. The Phase 3 study, slated to begin in late 2025, will further evaluate the safety, efficacy, and acceptability of the once-yearly formulation in larger, more diverse populations.
Dr. Jared Baeten, Senior Vice President and Virology Therapeutic Area Head at Gilead Sciences, emphasized the importance of this innovation: “Gilead is committed to developing person-centered HIV prevention options that meet the diverse needs of individuals at risk. Once-yearly lenacapavir, if approved, could become a critical tool in reducing new HIV infections worldwide.”
A future without HIV?
While there is currently no cure for HIV or AIDS, advancements like once-yearly lenacapavir represent a significant step forward in the fight against the epidemic. By offering a long-acting, highly effective PrEP option, Gilead aims to address barriers to adherence and persistence, ultimately helping to reduce the global burden of HIV.