HQ Team
October 17, 2024: Blood pressure measurement is a critical procedure in diagnosing and managing hypertension, yet it is fraught with scientific debates and controversies. These discussions revolve around the accuracy of measurement techniques, the interpretation of results, gender-based evaluation, and evolving treatment guidelines.
Added to these scientific measurement controversies is the emotional toll that a visit to a health facility and clinic entails. I suffer from white-coat hypertension, or a heightened blood pressure when visiting a doctor. Others routinely suffer from elevated blood pressure or constant ups and downs.
Blood pressure history
Blood pressure was measured for the first time in 1733 by Stephen Hale. He tied up a mare, cut open its crural artery, and inserted a pipe in it. He noticed that the blood that rushed up the tube oscillated up and down with each heart beat.
In 1881, Siegfreid Karl Ritter von Basch made the next great advance in blood pressure measurement that did not require one to cut open an artery. He created a machine that used an inflatable bag to compress the artery from the outside and measure the pressure when the blood flow was halted.
In 1905, Nikolai Korotkoff used the stethoscope and sphygmomanometer to listen to the artery being compressed to determine both the systolic and diastolic blood pressure of the patient. This method is largely unchanged and has become the gold standard of blood pressure measurement.
Is it good or bad?
Once humans learned to measure blood pressure without harm, the next debate was whether it should become a part of clinical diagnosis. And not strangely it was the health insurance companies that pushed for blood pressure measurement to become a part of clinical health declaration. This was because it was noticed that people with high blood pressure died early.
But the medical fraternity was not convinced and rooted for maintaining the status quo. Some believed that high blood pressure meant that it helped the blood move through clogged arteries and was in fact a good sign.
“The greatest danger to a man with high blood pressure lies in its discovery, because then some fool is certain to try and reduce it.”
– JH Hay, British Medical Journal 1931
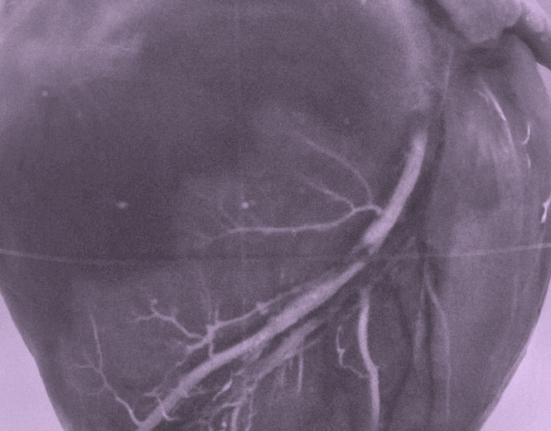
But soon better sense prevailed and studies were undertaken to determine the detrimental effect of blood pressure. The Framingham Heart Study was launched nearly 70 years ago (which is still ongoing with descendants of the original participants taking part) to study heart disease. The study zeroed in on “risk factors” for heart disease and one factor was blood pressure along with smoking, diabetes, and cholesterol. Importantly it reversed the order of belief by proving that blood pressure caused heart disease rather than the other way round.
Hypertension hype or fact
Now we come to the most crucial point of the matter, that is, the debate around measurement variables and the number that determine your hypertension.
This controversy is compounded by differences in how hypertension is experienced and diagnosed across genders, geographic locations, and various demographic factors.
The American Heart Association’s 2017 guidelines lowered the threshold for hypertension diagnosis to 130/80 mm Hg, down from 140/90 mm Hg. This change led to a substantial increase in the number of individuals classified as hypertensive, particularly affecting older adults who previously fell into the “normal” range.
The SPRINT trial supported this shift. However, other studies, such as ACCORD, did not find significant benefits from more aggressive treatment, leading to ongoing debates about management of the disease.
Differences in hypertension
Research indicates that men and women may experience hypertension differently. Men often develop hypertension at a younger age and have higher rates of severe hypertension compared to women. However, women tend to have a higher prevalence of hypertension post-menopause due to hormonal changes.
Additionally, treatment responses can vary; for instance, certain antihypertensive medications may be more effective in one gender over another. This necessitates gender-specific considerations in both diagnosis and treatment protocols.
Geographic variability
Geographic location significantly influences blood pressure levels and prevalence. Factors such as diet, lifestyle, healthcare access, and socioeconomic status contribute to these differences. For example, populations in regions with high sodium intake or low physical activity levels tend to have higher rates of hypertension. Moreover, cultural attitudes towards health and wellness can affect how individuals perceive and manage their blood pressure.
Socioeconomic factors play a crucial role in hypertension management. Individuals from lower socioeconomic backgrounds may face barriers such as limited access to healthcare, lack of education about health issues, and unhealthy lifestyle choices that can exacerbate hypertension.
Measurement errors
Accurate blood pressure measurement is critical but often flawed due to factors like “white coat syndrome,” where anxiety during clinical visits leads to elevated readings. Additionally, improper cuff size or placement can result in significant inaccuracies. These measurement errors can lead to misdiagnosis or inappropriate treatment decisions.
As guidelines continue to change based on emerging evidence, one thing is clear. There is a sweet spot for determining the correct measurement for hypertension and research shows it lies somewhere between 130 and 140 mm Hg. It is essential for healthcare providers to consider the above-mentioned diverse factors of gender, socioeconomic status, lifestyle, etc when diagnosing and treating hypertension.