HQ Team
August 18, 2025: An implant called TAR-200 has shown remarkable results in treating high-risk bladder cancer. According to a recent Phase 2 clinical trial data, the miniature pretzel-shaped device eliminated tumors in 82% of patients with high-risk non-muscle-invasive bladder cancer (NMIBC) who were unresponsive to bacillus Calmette-Guérin (BCG) therapy.
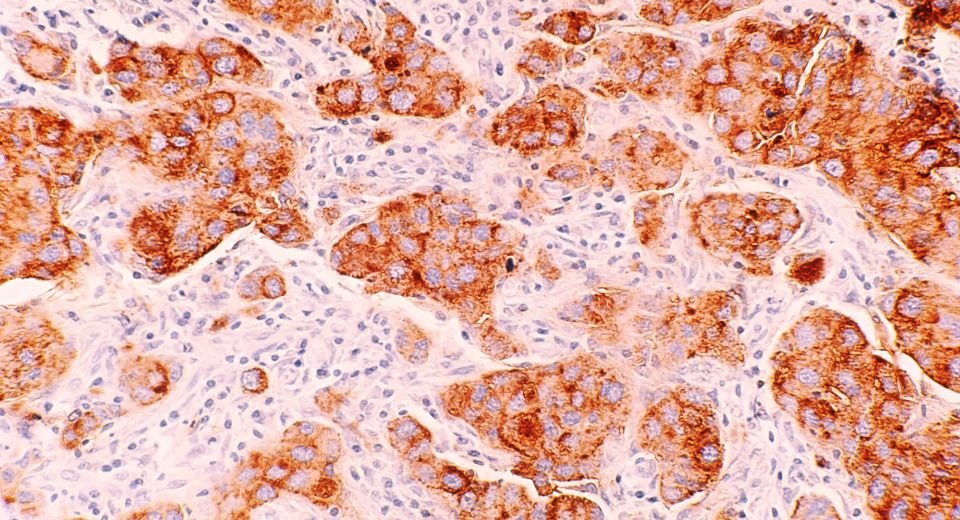
TAR-200 is a novel drug-device combination that slowly releases the chemotherapy drug gemcitabine into the bladder. Inserted via a catheter, it releases the drug consistently over a three-week treatment cycle. Unlike traditional liquid gemcitabine solutions, which remain in the bladder for only a few hours, TAR-200 provides sustained drug delivery, allowing the medication to penetrate deeper into the bladder tissue and destroy cancer cells more effectively.
The Phase 2b SunRISe-1 study included 85 patients with BCG-unresponsive high-risk NMIBC. Results showed that 70 out of 85 patients achieved complete remission (CR), with 45.9% remaining cancer-free at 12 months. The median time to achieve CR was 2.8 months, and 95.7% of patients achieved CR within the first three months. The treatment was well-tolerated, with most adverse events being mild urinary symptoms such as frequent urination, dysuria, and urinary urgency.
The SunRISe-1 trial was conducted at 144 locations worldwide, including Keck Hospital of USC. Researchers treated patients with TAR-200 every three weeks for six months, followed by four treatments annually for the next two years. The trial demonstrated that TAR-200 not only achieved a high complete response rate but also showed sustained efficacy, with 52.4% of responders remaining cancer-free at 12 months and 44.7% at 24 months.
TAR-200 implant
Non-muscle-invasive bladder cancer is the most common form of bladder cancer. While BCG immunotherapy is the standard treatment, it fails in 30-40% of patients, who then face the risk of disease recurrence or progression. Radical cystectomy (bladder removal surgery) is typically the primary treatment option for such patients. However, this surgery is highly invasive and carries significant health risks, potentially impacting patients’ quality of life. TAR-200 offers these patients a new non-surgical treatment option that preserves the bladder.
TAR-200 is designed to be implanted in a physician’s office in a 3- to 5-minute procedure without anesthesia. It remains in the bladder without interfering with daily activities and provides continuous drug delivery. In December 2023, the U.S. Food and Drug Administration (FDA) granted TAR-200 Breakthrough Therapy Designation for the potential treatment of BCG-unresponsive high-risk NMIBC patients ineligible for or unwilling to undergo radical cystectomy.
“Traditionally, these patients have had very limited treatment options. This new therapy is the most effective one reported to date for the most common form of bladder cancer,” said Sia Daneshmand, MD, director of urologic oncology with Keck Medicine of USC and lead author of the study detailing the clinical trial results published in the Journal of Clinical Oncology. “The findings of the clinical trial are a breakthrough in how certain types of bladder cancer might be treated, leading to improved outcomes and saved lives.”
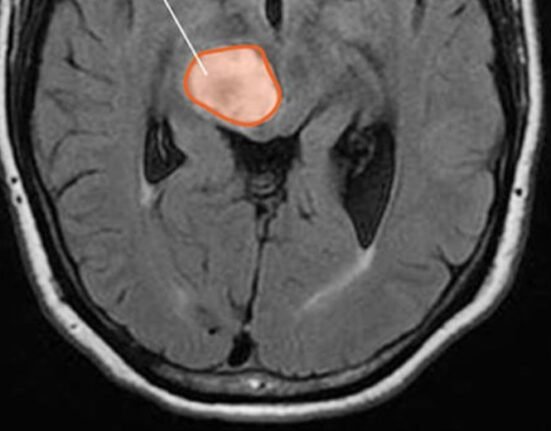
Bladder cancer care
Bladder cancer ranks among the top ten most common cancers worldwide, affecting nearly a million people each year. Despite advancements, the standard of care has remained largely unchanged for over 40 years, leaving patients with limited treatment options if initial BCG therapy does not work.
Bladder cancer is the sixth most common cancer in the U.S., with over 83,000 new cases diagnosed annually. TAR-200’s promising results mark a significant advancement in bladder cancer treatment, offering hope for patients and potentially transforming the treatment landscape.