By K. Leelamoni
December 12, 2023: The Human Papilloma Virus (HPV) is the name of a group of viruses of 200 known viruses.
They do not cause concern in most people, but infection with some high-risk types is common and can cause genital warts and cancer.
HPV infection causes about five percent of all cancers globally and also nearly all cervical cancers are found to be related to HPV.
Cervical cancer was the fourth leading cause of cancer and cancer deaths in women in 2020.
The highest prevalence of cervical HPV among women is in Sub-Saharan Africa, Latin America, Eastern Europe and Southeast Asia.
Cervical cancer
Cervical cancers account for 93% of HPV-related cancers in women. The highest rates of cervical cancer incidence and mortality are in low and middle-income countries.
In men, HPV infection tends to manifest clinically as anogenital warts and may later on lead to cancer in these areas. HPV infections are also associated with oropharyngeal cancers.
In India, current estimates indicate that every year 123,907 women are diagnosed with cervical cancer and 77,348 die from the disease.
Cervical cancer ranks as the second and most frequent cancer among women between 15 and 45 years of age in India.
Sexually transmitted
HPV is a common sexually transmitted disease and can affect the skin, genital area and throat.
Most people will not have any symptoms from an HPV infection. The immune system clears HPV from the body within a year or two with no lasting effects. Sometimes warts in the genital area may be painful or will bleed.
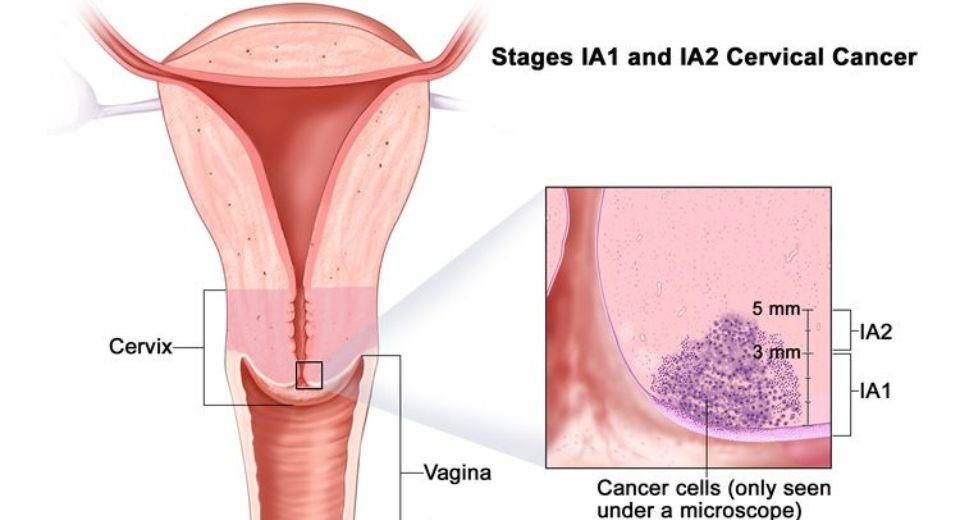
If the infection does not go away on its own, it can cause changes in cervical cells which lead to precancerous changes resulting in cervical cancer if left untreated.
It takes about 15-20 years for cervical cancer to develop after HPV infection. The symptoms may include bleeding between periods or foul-smelling vaginal discharge.
Currently, there is no specific treatment for HPV infection. Treating genital warts, cervical pre-cancers and cervical cancers is the only existing treatment option.
Vaccination
Being vaccinated is the best way to prevent HPV infection, cervical cancer and other HPV-related cancers. The vaccine is estimated to prevent up to 90% of cancers caused by HPV and genital warts.
Regardless of their gender, anyone can develop HPV-related cancers, so it is important to vaccinate girls and boys.
Considering the magnitude of cervical cancer, the vaccine should be given to all girls aged 9-14 years, before they become sexually active and also to the age group of 15 -26 years.
It is not routinely recommended for those above 27 years. People in this age group are unlikely to benefit because they have likely been exposed to HPV already.
In a promising advance in its fight against cervical cancer, India has recently launched its first indigenous HPV vaccine Cervavac.
Serum Institute of India
The Serum Institute of India, Pune developed and manufactured this quadrivalent recombinant vaccine. Though initially, it is available in the private market, plans are already undertaken to provide it through the government health system.
The recommended vaccine schedule for Cervavac in the age group of 9-14 is a two-dosage schedule at zero and six months and a three-part dosage for 15-26 years of age at zero, two and six months.
The indigenous vaccine is made available in India at a comparatively low cost. The Union Health Ministry also intends to roll out the HPV vaccine against cervical cancer in the national immunisation programme for girls aged 9 -14 years and plans to provide it through schools.
I was happy to read recently, the news about the Indian Medical Association women’s wing, Kozhikode unveiling the HPV vaccine.
Awareness creation through health professionals, movie stars, media and other agencies is essential before implementing such programmes.
(The writer was a former Head of the Department of Community Medicine at the Government Medical College in Kozhikode and Thiruvananthapuram and worked at the Amrita Institute of Medical Sciences in Kochi.)








1 Comment