By Dr K. Leelamoni
October 16, 2023: Sheela, 19, a student studying medicine in India’s southern city of Thiruvananthapuram, was bitten by a stray pup at a hostel in the hospital.
She ignored the incident until she was down with a fever. Her friends took her to a hospital where she died due to rabies.
The incident, which took place in the late 1970s — when I had just joined the state’s community health system — left me with a sense of shock.
The stray dog menace still continues in Kerala state, of which Thiruvananthapuram is the capital.
Kerala faced a spurt in rabies and stray dog bites last year. There were 21 deaths and 1.96 lakh dog bites in the state in 2022.
Central nervous system
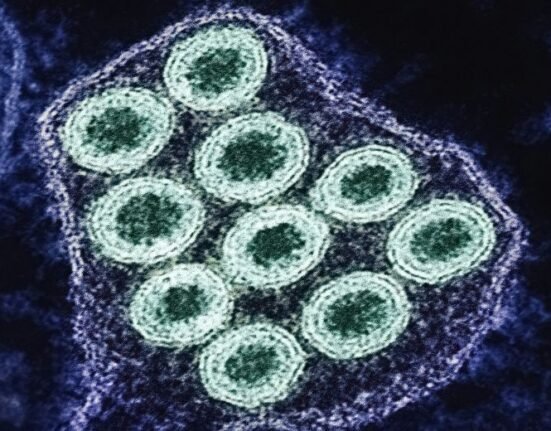
Dogs are the main sources of human rabies — a vaccine-preventable viral zoonotic disease — contributing to about 99% of cases and deaths.
The disease mainly affects the central nervous system. Once clinical symptoms appear, rabies is 100% fatal.
Rabies is transmitted through the saliva of a rabid animal through bites, licks on wounds, scratches, broken skin or mucous membranes of the mouth and nose.
India accounts for 36% of world rabies deaths. It causes 18,000-20,000 deaths a year in the South Asian nation.
Rabies is present in more than 150 countries. It is mainly prevalent in Asia and Africa. Of the total deaths globally, 40% are accounted for by children below 15 years.
‘Painful death’
Foxes, jackals, mongoose racoons and cats can also transmit the infection. Rarely bat transmission is reported. They are not spread by rodents.
I was an unfortunate witness to the horrible and painful death of Sheela. She showed intolerance when the fan was switched on and got agitated when given a glass of water.
The two symptoms revealed that she was in a critical stage of rabies — aerophobia (fear of air) and hydrophobia (fear of water) progressing to paralysis and death. In her case, these symptoms occurred after two months of being bitten.
After a bite, the virus enters through the peripheral nervous system at the site of the bite and migrates to the central nervous system. Clinical symptoms appear after an incubation period of 2-3 months of bite.
Once the symptoms appear there is no effective treatment and death occurs within 7-10 days.
Vaccines
Effective vaccines are available at present for both preventing the disease after a bite and for protection before exposure.
Wound treatment is the most effective first-aid treatment against rabies. Wash immediately with soap or detergents and flush the wound thoroughly for about 15 minutes.
This will help to wash away the saliva and the viral particles from the site of the bite before they get attached to the peripheral nerves.
Apply iodine-containing disinfectants and do not cover the wound with a dressing or bandage.
If possible observe the biting animal for 10 days.
If the animal is healthy and normal, the bite was provoked, and the animal is fully immunised then there is no need for a vaccination.
Vaccination of dogs, even puppies, is another step in prevention. It stops the transmission from the dog. Vaccinating 70% of dogs can break rabies transmission in high-risk areas.
1970s fear of vaccines
During post-exposure prophylaxis administration of a series of rabies vaccine injections on specified dates after the bite is vital.
Since the protective antibodies will appear only within 10 days, in severe cases, rabies immunoglobulin also should be given along with the first dose of the vaccine to provide immediate protection.
Pregnant and lactating women also can take vaccines safely.
I was thinking of the days years ago when we were working as junior faculty in the preventive clinics of medical colleges, the process of vaccination was much more traumatic than rabies itself.
We administered 10 ml of the old rabies vaccine subcutaneously (beneath the skin) around the umbilicus for 14 days for adults.
Intradermal vaccines
Very often they stop coming after a few days due to the pain and redness in the area. The cases of children were more traumatic.
In the state’s northern Kozhikode Medical College, usually children, even infants were brought after jackal bites from places like neighbouring Wayanad district with severe bites on the face and head.
Today we have very effective vaccines against rabies. Usually, the dosing schedule is five doses of 1 ml intramuscularly (0,3,7,14,28th day). Zero is the day when the first dose is given.
The vaccine is also now given intradermally, done within or between the layers of skin. Since the dose is only 0.1 ml, the amount of vaccine needed is less and hence the cost is also less.
Knowing well that the efficacy and safety of both vaccines remain the same and I can treat the disease, there is still a hesitancy within me to cross a path where a pack of dogs roam around.
At times I stop and observe to make sure I am 100% on the safe side.
After seeing too many cases of dog bites and their consequences I guess I will always remain apprehensive.
(The writer was a former Head of the Department of Community Medicine at the Government Medical College in Kozhikode and Thiruvananthapuram and worked at the Amrita Institute of Medical Sciences in Kochi.)







2 Comments