HQ Team
November 5, 2025: A new study reveals that initiating statin therapy within three years of an early-stage breast cancer diagnosis can significantly reduce mortality, offering new hope for patients. This research adds to a growing body of evidence that these commonly prescribed cholesterol-lowering medications may have powerful anti-cancer properties that could enhance survival rates for breast cancer patients.
Danish researchers say statin therapy after a breast cancer diagnosis is associated with clinically meaningful improvements in survival. The study analyzed data from 66,952 women with stage I-III breast cancer diagnosed between 2000 and 2021 using an advanced statistical method called “target trial emulation” that mimics randomized controlled trials.
The key findings from this extensive research revealed that patients who started statins within three years of diagnosis had a 10% lower risk of dying from breast cancer and an 8% lower risk of dying from any cause compared to non-users. The 10-year risk for breast cancer mortality was 11.8% among statin initiators versus 13.5% among noninitiators – a difference of 1.7%.
Perhaps most notably, researchers calculated that only 59 patients would need to take statins to prevent one additional breast cancer death at 10 years, indicating a meaningful clinical benefit. The survival advantage was most pronounced in women who started statins sooner after diagnosis, with those initiating statins within 12 months showing a remarkable 28% lower risk of breast cancer mortality.
“Clinically, this means that if a patient is prescribed statins after diagnosis for cardiovascular reasons, there is no reason to stop them — in fact, there may be added benefit,” stated lead author Dr. Sixten Harborg of Aarhus University Hospital.
Mounting evidence
The Danish research aligns with several recent meta-analyses that have pooled data from multiple studies to identify statistically significant protective associations between statin use and breast cancer outcomes:
-
A June 2025 meta-analysis published in the British Journal of Cancer that included nearly 700,000 breast cancer cases found statin use was associated with an approximately 20% reduction in both breast cancer mortality and recurrence risk.
-
The same analysis revealed that lipophilic statins (such as atorvastatin, simvastatin, and lovastatin) demonstrated stronger protective effects against breast cancer death than hydrophilic statins.
-
Earlier research published in the International Journal of Cancer found statin use was associated with improved recurrence-free survival , with benefits confined specifically to lipophilic statins.
-
A 2015 meta-analysis in Oncotarget reported significant negative associations between both pre-diagnosis and post-diagnosis statin use and breast cancer mortality .
This accumulating evidence strongly suggests the relationship between statin use and improved breast cancer outcomes is consistent across diverse patient populations and study methodologies.
How statins fight cancer
Researchers have identified several plausible biological mechanisms through which statins may exert anti-cancer effects:
-
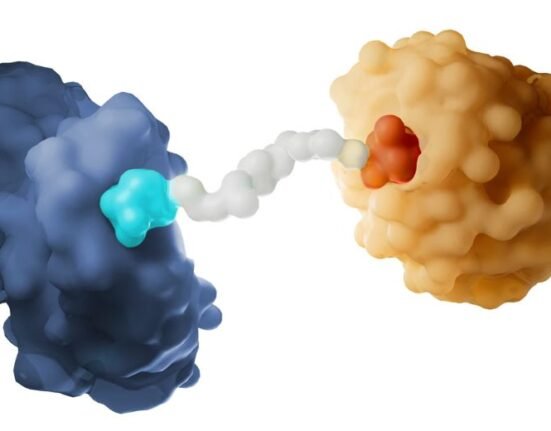
Cholesterol pathway inhibition: Statins work by inhibiting HMG-CoA reductase, the rate-limiting enzyme in the cholesterol synthesis pathway. This enzyme is overexpressed in breast cancers, making it a promising therapeutic target.
-
Tumor growth suppression: By blocking the mevalonate pathway, statins deplete tumor cells of cholesterol and isoprenoids needed for cell membrane synthesis and rapid proliferation .
-
Apoptosis induction: Statins can trigger programmed cell death in cancer cells through multiple pathways, including activation of c-Jun NH2-terminal kinase.
-
Metastasis inhibition: Statins reduce cancer’s ability to spread by blocking processes essential for invasion and migration, including RhoA cell-signaling pathways and matrix metalloproteinase expression.
-
Immunomodulatory effects: Beyond direct anti-tumor activity, statins influence immune responses that may enhance the body’s ability to fight cancer.
Lipophilic vs. Hydrophilic statins
Emerging evidence suggests that lipophilic statins may be more effective against breast cancer than their hydrophilic counterparts. This distinction appears logical from a biological perspective – lipophilic statins can more easily penetrate cell membranes throughout the body, while hydrophilic statins are more liver-specific .
The British Journal of Cancer meta-analysis confirmed this difference, showing lipophilic statins had more protective effects against breast cancer death than hydrophilic statins . This echoes preclinical studies that have demonstrated superior anti-proliferative effects of lipophilic statins on breast cancer cells .
Common lipophilic statins include atorvastatin, simvastatin, lovastatin, and fluvastatin, while pravastatin and rosuvastatin are classified as hydrophilic.
While the evidence is compelling, experts emphasize important nuances in interpreting these findings. They caution that despite encouraging results, statins are not yet recommended as standard breast cancer treatment outside their approved cardiovascular indications. For patients already taking statins for cholesterol management when diagnosed with breast cancer, the research strongly supports continuing this medication rather than discontinuing it.
Dr. Naomi Ko, a medical oncologist at NYU Langone Perlmutter Cancer Center, noted that treatment decisions should be personalized, considering that “the group that had the statins already had better prognosis, given that they had smaller tumors and lower grade tumors”.
Since aromatase inhibitors used in breast cancer treatment can raise cholesterol levels, monitoring and appropriate statin initiation when indicated is recommended.
The ongoing MASTER trial (MAmmary cancer STatins in ER positive breast cancer) represents a crucial next step in validating these observational findings. This double-blind, phase III, randomized, controlled trial is investigating whether adding atorvastatin (80 mg/day) to standard therapy improves outcomes for women with early-stage, estrogen receptor-positive breast cancer -5.
“As we wait for randomized trial data from the MASTER trial, the results are encouraging,” noted Dr. Harborg, reflecting the research community’s cautious optimism about statins’ potential in oncology .
The trial, which aims to enroll 3,360 patients, will specifically examine whether statin therapy can reduce the risk of recurrence in this patient population. If successful, it could pave the way for statins to be repurposed as a safe, well-tolerated, and inexpensive adjunctive treatment for breast cancer.
The accumulating evidence from recent studies provides a strong foundation for considering statins’ potential role in improving breast cancer outcomes. While not yet sufficient to recommend statins universally for breast cancer patients without cardiovascular indications, the research clearly demonstrates that these medications may offer dual benefits for appropriate patients.