HQ Team
April 17, 2025: Stem cell therapies, which replace dead cells in the brain, can stop movement problems, rigidity and tremors in patients with Parkinson’s disease, two small trial studies show.
The cells are injected into the brain and could replace the nerve cells that die. Once injected, these stem cells become specialised neurons that release dopamine, which coordinates the movement, according to the studies published in Nature.
In the Memorial Sloan Kettering Cancer Center study, nerve cells (neurons) derived from embryonic stem cells were transplanted into the brains of 12 Parkinson’s patients to produce dopamine.
Parkinson’s patients have unusually low levels of dopamine, and as a result, suffer from tremors, slowness, stiffness, and walking or balance problems.
Cell replacement provides a completely new treatment modality compared to the currently available treatments, said neurologist and researcher Ole Isacson of Harvard Medical School and McLean Hospital in Belmont, Mass., who was not involved in the trials.
Levodopa
Traditional treatments like levodopa offer only temporary symptomatic relief but may cause dyskinesia. Early fetal tissue therapies demonstrated long-term benefits but were constrained by ethical and supply issues.
During the early phase of the Memorial Sloan Kettering clinical trials, the researchers reprogrammed patients’ own stem cells to replace dopamine neurons in the brain. It treated three of six participants who will be tracked for more than a year.
The goal of the trial was to test the safety of the procedure and monitor for any improvements in Parkinson’s disease. Following the first six patients transplanted in the phase 1 study, the researchers hope to expand and recruit more patients as part of a mid-stage study.
“Safety data through 18 months continued to indicate a favourable safety profile. The treatment process, including surgery and immunosuppression, was generally well tolerated,” the researchers wrote.
People’s own cells
The transplantation approach of using a person’s own cells circumvents the requirement for immunosuppressive treatments, which are necessary when cells from other donors are used.
“We believe this approach may open up a new treatment paradigm and lead to the development of many additional cell therapies to restore damaged brain systems and replace degenerated brain cells in other diseases,” said Isacson, who heads McLean Hospital’s Neuroregeneration Research Institute.
In the second study, seven patients with Parkinson’s, aged between 50 and 69, participated in an open-label trial.
The first patient initially received a unilateral transplant for an eight-month safety evaluation and received a second implant to complete the bilateral treatment only after tolerability was confirmed.
The remaining six patients underwent concurrent bilateral transplants.
24-month follow-up
Over the 24-month follow-up, no serious adverse events were reported, according to the researchers.
In total, 73 mild to moderate events were observed, from injection-site itchiness to one moderate case of transient dyskinesia.
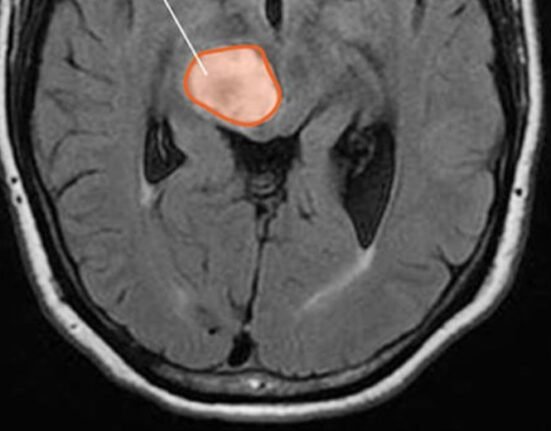
MRI scans revealed a gradual increase in graft volume, reflecting the normal distribution and spread of the transplanted cells rather than any uncontrolled or abnormal growth.
“Four out of six patients improved by up to 20% in motor scores off medication, while on medication, performance improved by an average of 4.3 points —demonstrating enhanced movement control from the transplanted cells.”
As of December, there were 115 clinical trials underway for 83 products derived from pluripotent stem cells3.
Fetal tissue
Past trials using fetal tissue as a source of dopamine neurons had problematic side effects, mainly involuntary movement called graft-induced dyskinesia.
“We were naturally concerned about dyskinesia and looked very carefully for it in our trial,” Lorenz Studer, MD, Director of MSK’s Center for Stem Cell Biology, who developed the cell therapy for the Memorial Sloan Kettering study.
“One of the very gratifying results was that we didn’t see any evidence with our treatment. Overall, there were no serious side effects from the transplanted cells or immunosuppression.”
‘Important step forward’
Treatments for Parkinson’s disease are at a more advanced stage of development than are those for any other central nervous system disease, said Hideyuki Okano at the Keio University Regenerative Medicine Research Center, Kawasaki.
“The fact that both independent trials proved to be safe and hinted at possible efficacy is an important step towards the establishment of this cell therapy for Parkinson’s disease in wider society.
“The next stages of clinical trials, phases II and III, are awaited to fully assess the efficacy of these interventions,” he said.