HQ Team
January 31, 2025: Britain’s National Health Service will provide a gene therapy that may cure sickle cell disease for patients 12 years and older, according to a National Institute for Health and Care Excellence (NICE) statement.
The one-off gene therapy, known as exagamglogene autotemcel (or ‘ex-cell’), has been approved for use on the NHS in England from January 31, 2025, by the NICE for older children and adults with a severe form of sickle cell disease.
Clinical trials suggest exa-cel can stop painful and unpredictable sickle cell crises – the most common symptom of sickle cell disease – where blood vessels become blocked, causing severe pain, with experts saying the therapy offers patients a chance of disease-free life.
Researchers concluded there was a ‘functional cure’ in 96.6% of exa-cel trial participants who received it, according to the statement.
In clinical trials, all patients who received exa-cel also avoided hospitalisation for a year following treatment – and almost 98% had still avoided hospitalisation around 3.5 years later.
Vertex Pharmaceuticals
The therapy from Vertex Pharmaceuticals and CRISPR Therapeutics will cost the state-funded NHS about 1.65 million pounds ($2.1 million) a course. The medicine is being manufactured in the UK, near Edinburgh.
On January 31, 2025, Vertex announced a reimbursement agreement with NHS England. The administration of the therapy requires experience in stem cell transplantation and the management of hemoglobinopathies. Therefore, Vertex is continuing to engage with experienced hospitals throughout England to establish a network of independently operated authorized treatment centers.
Britain’s Medicines and Healthcare Products Regulatory Agency in 2023 became the first in the world to approve the therapy, which uses gene-editing tool CRISPR.
NICE ensures that the healthcare workforce of the NHS has the right numbers, skills, values and behaviours to support the delivery of excellent healthcare and health improvement to patients and the public.
It also works with the wider NHS and its partners to optimise the use of digital technology, research and innovation and to deliver value for money and increased productivity and efficiency.
‘Revolutionary gene therapy’
The NHS is a publicly funded healthcare system in England and is the second largest single-payer healthcare system in the world after the Brazilian Sistema Único de Saúde.
“This innovative, gene-editing therapy offers hope of a cure for people facing a severe form of the disease and could be transformative – it could enable patients to live free from the fear of sickle cell crises hanging over them,” said Amanda Pritchard, chief executive of the NHS.
“It is just the latest in a series of revolutionary gene therapies NHS England has secured for patients, and we are funding this new treatment option straight away so patients can benefit from the enhanced quality of life it offers,” she said.
Sickle cell disease, before this therapy, required lifelong treatment regimens, greatly impacting the quality of life, with people suffering from chronic pain, fear of sickle cell crises, hospitalisation, and shortened life expectancy, and many patients describe it as ‘looming over their daily lives’.
Stem cell transplant
According to NHS data, there were just over 32,000 hospital admissions in England in 2023-24 for sickle cell disorders. Almost 14,000 of these admissions were admissions for sickle cell anaemia crises.
The treatment will be offered at specialist NHS centres in London, Manchester and Birmingham, and follows a deal in August 2024 for the NHS to access exa-cel for eligible patients with transfusion-dependent beta-thalassaemia.
It will be available for eligible patients who are 12 years and older and who experience recurrent sickle cell crises and would be suitable for a stem cell transplant but where a donor is not available.
Gene mutation
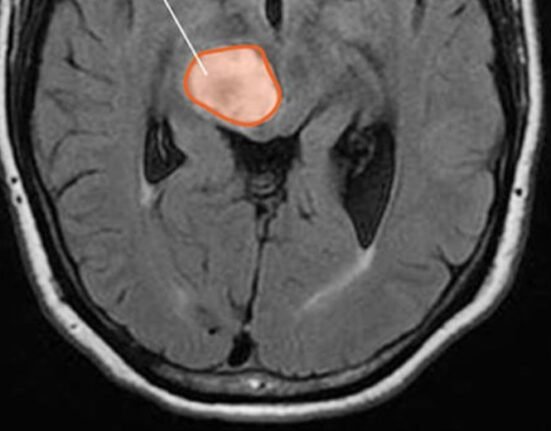
In sickle cell disease, a gene mutation causes red blood cells to become irreversibly sickle-shaped, which can lead to haemolytic anaemia – a blood condition that occurs when your red blood cells are destroyed faster than they are replaced.
Over a long period, the disorder can cause severe organ damage and intense pain if damaged red blood cells block vessels and restrict oxygen supply, which can also lead to strokes and heart failure.
Exa-cel uses CRISPR technology to enable the editing of a gene in a patient’s bone marrow stem cells so that the body produces functioning haemoglobin.
Blood stem cells are removed from a patient’s body and edited in a laboratory using CRISPR technology. The treated cells are then returned to the patient via an infusion.