HQ Team
November 22, 2024: Researchers at the University of California, San Diego, have developed a wearable ultrasound patch that continuously monitors blood pressure. This device, roughly the size of a postage stamp, has shown promising results in clinical trials involving over 100 patients.
Key features of the wearable patch
Unlike traditional cuff-based devices that provide isolated readings, the patch offers a continuous stream of blood pressure waveform data. This allows for the identification of critical trends and fluctuations in blood pressure levels.
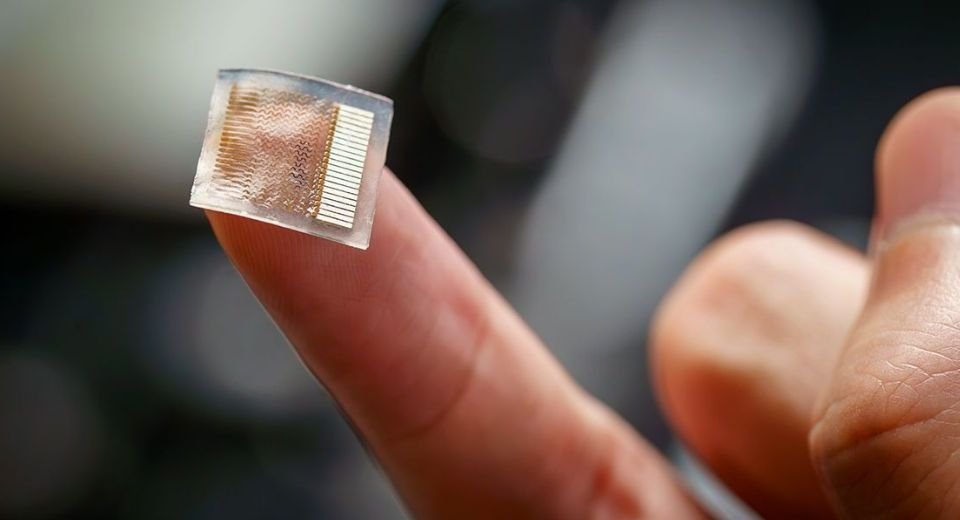
The soft, stretchy patch adheres to the skin on the forearm and utilizes an array of tiny transducers to send and receive ultrasound waves. These waves track changes in blood vessel diameter, converting them into accurate blood pressure readings.
In tests with patients in intensive care and those undergoing cardiac procedures, the patch’s measurements closely matched those taken from invasive arterial lines, demonstrating its potential as a reliable non-invasive alternative.
To further test its accuracy, the patch was tested while people went about their daily activities such as cycling, sitting and standing or even meditating. In all cases, readings closely matched those from blood pressure cuffs. “Blood pressure can be all over the place, depending on factors like white coat syndrome [being in a doctor’s office], masked hypertension, daily activities or use of medication, which makes it tricky to get an accurate diagnosis or manage treatment,” said Sheng Xu, a professor of chemical and nano engineering at UC San Diego who developed the patch. “That’s why it was so important for us to test this device in a wide variety of real-world and clinical settings.”
Benefits of continuous BP monitoring
Maintaining normal blood pressure (120/80 mmHg) is crucial for preventing serious health issues such as heart disease, stroke, and kidney problems. Traditional methods often miss critical patterns due to their one-time measurement approach. The wearable patch addresses this gap by providing real-time data that can help manage hypertension more effectively.
The development of this wearable patch is part of a broader trend in blood pressure monitoring technology. Here are some notable innovations:
Cuffless Devices: New technologies are emerging that eliminate the need for inflatable cuffs. These devices can measure blood pressure continuously or on demand through various methods, including photoplethysmography (PPG) and electrocardiography (ECG).
Smartphone Integration: Applications like OptiBP™ use smartphone cameras to measure blood pressure at the fingertip, making monitoring more accessible without traditional hardware.
AI and Machine Learning: The integration of AI enhances the accuracy and functionality of wearable monitors by analyzing large datasets to identify patterns and predict health issues related to hypertension.
Future directions
The research team at UC San Diego plans to refine the wearable patch further and conduct large-scale clinical trials. As wearable technology continues to evolve, it holds great promise for improving hypertension management and overall patient outcomes by providing more comprehensive health data in real-world settings.
However, there are certain hesitations and concerns about adopting cuffless blood pressure measuring devices. “Unfortunately, the pace of evidence, regulation and validation testing has lagged behind the pace of innovation and direct consumer marketing,” write Stephen P. Juraschek, physician investigator at Beth Israel Deaconess Medical Center in Boston, and colleagues in a review published in Current Cardiology Reports. There are no guidelines yet monitoring their use by regulatory bodies, though the European Society of Hypertension has said that cuffless devices should not be used to make diagnostic or treatment decisions.
The study was published in the journal Nature Biomedical Engineering.