HQ Team
December 5, 2023: The response of immune cells inside the protective covering of the brain may lead to a cognitive decline in people with chronic high blood pressure, a study on mice finds.
“The role of immune signalling in cognitive decline is critically important to understand,” said Roderick Corriveau, PhD, program director, National Institute of Neurological Disorders and Stroke.
“These findings offer insight into how signalling from the immune system could contribute to symptoms of cognitive decline that ultimately result in dementia diagnoses.”
Hypertension or high blood pressure is when the pressure in your blood vessels is too high (140/90 mmHg or higher).
About 1.28 billion adults aged 30–79 years worldwide have hypertension, and two-thirds are living in low- and middle-income countries.
46% unaware
An estimated 46% of adults with hypertension are unaware that they have the condition and less than half of adults (42%) with hypertension are diagnosed and treated, according to the WHO.
The study on hypertension in mice, supported by the National Institutes of Health NIH), suggested that immune cells around and within the brain become abnormally activated under conditions that mimic a common form of hypertension, and this activation leads to impaired brain function.
The researchers led by Costantino Iadecola, MD, director and chair of the Feil Family Brain and Mind Research Institute, New York City, found abnormally increased levels of interleukin-17 — a chemical normally released in the body to activate the immune system — in the cerebral spinal fluid and the brain.
Dr Iadecola’s team previously showed that a high salt diet increased IL-17 in the gut, which was followed by cognitive impairment.
“The new findings add to that story by showing that IL-17 is acting within the brain itself,” according to a statement from the US national medical research agency, NIH.
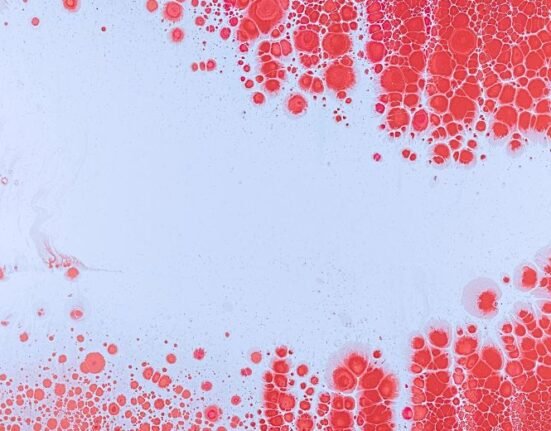
Macrophages
Once in the brain, IL-17 turns on immune cells responsible for activating inflammation and fighting off infections, known as macrophages.
A series of experiments confirmed that these macrophages are important for the observed decline in cognition.
Both the categories of mice, one in which the receptor for IL-17 was deleted in brain macrophages and those that had their brain macrophages depleted, showed no effects of high blood pressure on cognitive function despite having other symptoms of hypertension.
“This is currently the most realistic model of hypertension that we have,” said Dr Iadecola. “The (salt model) DOCA mouse simulates low-renin hypertension, which is a common type of hypertension in people, particularly among Black Americans.”
The researchers’ initial hypothesis was that the gut releases IL-17, which then travels to the brain through the bloodstream.
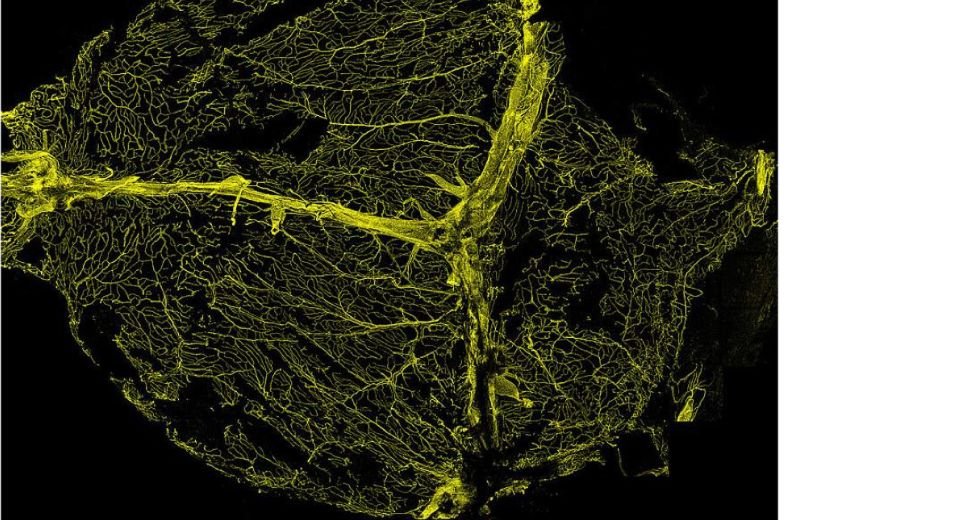
Meninges
Once there, it sets off a reaction that damages the ability of brain blood vessels to respond appropriately to increased brain activity.
However, blocking the brain blood vessels’ ability to respond to IL-17 only partially rescued cognitive impairment, suggesting that there was another source of IL-17 acting on the brain.
Barriers exist within the protective covering of the brain, called the meninges, to prevent unwanted spillage into the brain.
“However, this barrier appeared to be disrupted in the mice with experimentally induced hypertension, and this disruption allowed IL-17 to enter the cerebral spinal fluid,” according to the statement.
The researchers stated that targeting T cells — a type of white blood cell called lymphocytes — which help the immune system fight germs and protect from disease could be a new treatment approach.
“Together, our data suggest two different effects are caused by hypertension,” said Dr Iadecola. “One is IL-17 acting on blood vessels, but this appears to be relatively minor.”
“A more prominent, central effect is caused by cells in the meninges releasing IL-17 that directly affects immune cells in the brain.
“It is these immune cells, activated by signaling from the meninges, that ultimately affect the brain in a way that causes cognitive impairment.”