HQ Team
October 6, 2024: The Democratic Republic of the Congo has started mpox vaccination aiding efforts to halt the spread of the viral disease, according to the World Health Organization.
The central African nation began the campaign in the eastern North Kivu province, and it will be subsequently rolled out in 11 of the most affected regions of Equateur, North Kivu, Sankuru, South Kivu, Sud-Ubangi and Tshopo provinces, according to a WHO statement.
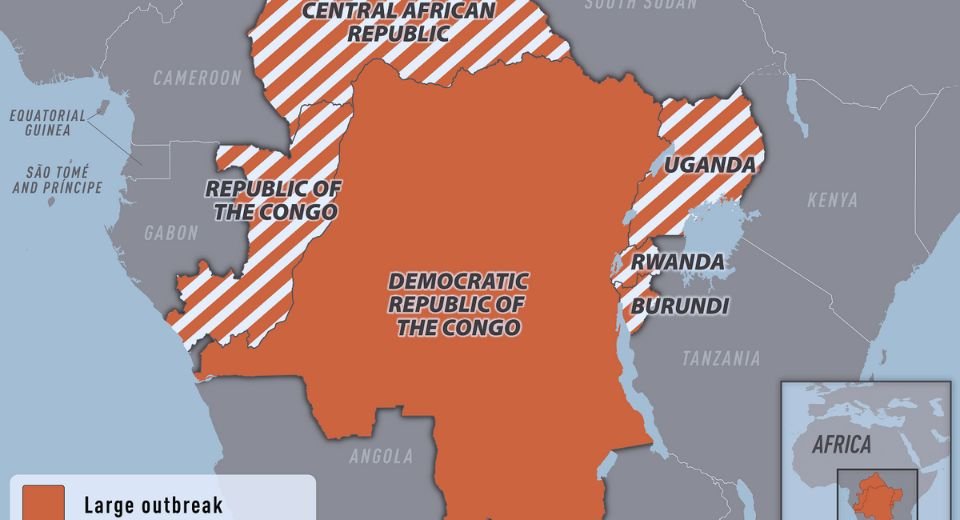
Congo has reported more than 30,000 suspected and laboratory-confirmed cases, and 990 deaths since the start of 2024 – accounting for 90% of the cases reported from 15 countries in the African region so far this year.
It has received 265,000 doses of the MVA-BN vaccine donated by the European Commission’s Health Emergency Preparedness and Response Authority, Gavi, the Vaccine Alliance, and the United States Government.
In September 2024, WHO added the MVA-BN as the first mpox vaccine to its prequalification list, a step that is expected to facilitate timely and increased access to this vital product in communities with urgent need, to reduce transmission and help contain the outbreak.
Delivery of vaccines
“As we rally efforts to stop the mpox outbreak, the rollout of the vaccine marks an important step in limiting the spread of the virus and ensuring the safety of families and communities,” said Dr Matshidiso Moeti, WHO Regional Director for Africa.
“Vaccines are an important additional tool in outbreak control and we’re grateful to our partners who have donated the doses. We’re working closely with the national authorities to effectively deliver the vaccines to those who need them most,” she said.
WHO recommends that vaccination be implemented as part of a comprehensive response that includes enhanced surveillance, community engagement, contact tracing, public health and social measures, and appropriate case management.
The WHO declared the mpox outbreak as a public health emergency of international concern in August. The move came after a new clade was detected and its rapid spread to neighbouring countries caused concern.
Caused by an orthopoxvirus, mpox was first detected in humans in 1970 in Congo. The disease is considered endemic to countries in Central and West Africa. Last year, reported cases increased significantly, and already, the number of cases reported so far this year has exceeded last year’s total.
300 WHO experts
WHO and partners are working closely with the national authorities to scale up and reinforce all the key control measures to save lives and end the outbreak, according to the statement.
More than 300 WHO experts supporting polio eradication efforts in Congo have been integrated into the mpox response.
The experts have extensive field experience in public health, particularly in community-based and health-facility active surveillance, case investigations, contact tracing and risk communication, and have been at the forefront of the fight against polio and other vaccine-preventable diseases, according to the statement.
As a part of preparations for the vaccination programme, WHO has supported the national health authorities in a range of areas, including training health workers; enhancing vaccine delivery systems and infrastructure such as vaccine storage and transportation; community engagement; as well as ensuring supervision and evaluation of the process for quality vaccine delivery.
Efforts are also ongoing to reinforce measures to identify and address vaccine mis- and disinformation and engage with community and religious leaders to increase access to accurate information, the WHO stated.
Sexual contact
Mpox vaccines are currently in short supply, especially in Africa.
WHO is working with partners, including Gavi, the Vaccine Alliance and UNICEF, to establish a distribution mechanism for doses being donated by other countries as well as from direct procurements from the vaccine manufacturer.
According to the Centres for Disease Control and Prevention, person-to-person transmission had occurred during this outbreak, including through sexual contact, day-to-day household contact, and within the healthcare setting— in the absence of appropriate personal protective equipment. There has also been transmission from contact with live or dead wild animals.