HQ Team
June 10, 2023:The Food and Drug Administration (FDA) has accepted an application for what could become the first-ever marketed medicine based on CRISPR gene editing technology. Developed by Vertex Pharmaceuticals and CRISPR Therapeutics, this innovative treatment targets two rare blood disorders: sickle cell disease and beta thalassemia.
The drug, known as exa-cel, has been granted a priority review for sickle cell disease, with a decision anticipated by December 8. Meanwhile, a standard review has been assigned for beta thalassemia, and the FDA aims to make a ruling by March 30, 2024. The treatment is the first of its kind to be brought to U.S. regulators and will be a test case for how the agency views the gene editing technology.
Researchers Emmanuelle Charpentier and Jennifer Doudna won a Nobel Prize in 2020 for CRISPR gene editing technology, and if FDA approves, it will open the gates for similar future approvals.
The companies have presented new results, for exa-cel from Phase 3 studies in sickle cell and beta thalassemia, which have met their pre-specified goals.
In the beta thalassemia study, 24 of 27 patients did not need blood transfusions for at least a year. Of the three who did, one could do without a transfusion for three months, while the two others reduced the need for blood volumes by 80% to 96%. In the sickle cell study, 16 of 17 patients haven’t had any pain crises for at least a year, with a mean duration of about 19 months and a maximum of 37 months.
The trial is designed to follow participants ( ages 2 to 11 years )for up to 15 years after exa-cel infusion.
These findings will be presented at the upcoming European Hematology Association meeting, generating further anticipation for the potential of CRISPR-based therapies in the field of blood disorders.
About exagamglogene autotemcel (exa-cel)
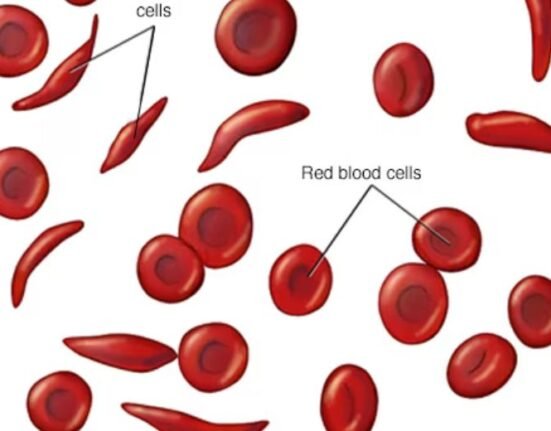
Exa-cel is an investigational CRISPR/Cas9 gene-edited therapy in which a patient’s own hematopoietic stem cells are edited to produce high levels of fetal hemoglobin (HbF; hemoglobin F) in red blood cells. HbF is the form of the oxygen-carrying hemoglobin that is naturally present during fetal development, which then switches to the adult form of hemoglobin after birth. The elevation of HbF by exa-cel has the potential to reduce or eliminate painful and debilitating VOCs for patients with SCD and alleviate transfusion requirements for patients with TDT.
Europe approval
In Europe, the Marketing Authorization Applications (MAAs) for exa-cel were submitted in December 2022 and validated by the European Medicines Agency (EMA) and the Medicines and Healthcare products Regulatory Agency (MHRA) in January 2023. In the EU, exa-cel has been granted Orphan Drug Designation from the European Commission, as well as Priority Medicines (PRIME) designation from the EMA, for both SCD and TDT, according to a press statement. In the U.K., exa-cel has also been granted an Innovation Passport under the Innovative Licensing and Access Pathway (ILAP) from the MHRA.