HQ Team
January 3, 2023: A team of researchers at Houston Methodist Hospital in the US have developed a small implant that can eliminate type 1 diabetes symptoms
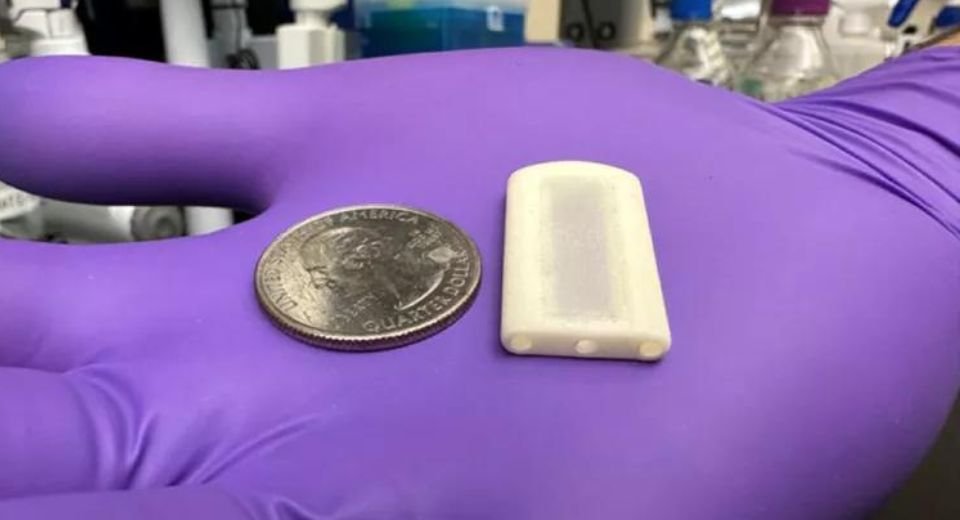
The experiment was carried out on rats, and human trials are awaited. The 3D-printed device called the Neovascularized Implantable Cell Homing and Encapsulation (NICHE), releases therapeutics into the body. The treatment restored healthy glucose levels and eliminated Type 1 diabetes symptoms in animal models for over 150 days. The researchers managed to curb the adverse effects of anti-rejection therapy by administering immunosuppressive drugs where the transplanted islet cells were located.
NICHE uses resins, tiny pores, and nanofluidics to keep the islet cells healthy while storing and releasing immunosuppressants.
Type 1 diabetes, is caused by the body’s immune system attacking and destroying cells in the pancreas, which make insulin. Without enough insulin, blood sugar levels shoot up, causing a variety of side effects. In severe cases, people may need pancreas or liver transplants.
In severe cases, patients may need an islet cell transplant, where the islet cells of a deceased pancreas donor are harvested, processed and then transplanted into the Type 1 diabetes patient’s liver. But this requires using immunosuppressant drugs for the rest of their lives to avoid transplant rejection.
It is the first time direct vascularisation and local immunosuppression have been combined into a single, implantable device for long-term Type 1 diabetes management. The team said direct vascularisation is fundamental for supplying nutrients and oxygen for maintaining the viability of transplanted islet cells.
“A key result of our research is that local immunosuppression for cell transplantation is effective,” says corresponding author Dr Alessandro Grattoni, chair of the Department of Nanomedicine at Houston Methodist Research Institute.
“This device could change the paradigm of how patients are managed and can have a massive impact on treatment efficacy and improvement of patient’s quality of life.”
The NICHE requires drug refilling every 28 days, comparable to other long-acting drugs that are clinically available.
Grattoni’s team is working on scaling up the NICHE technology for clinical deployment, for which drug refilling may only be needed once every six months.
Next, the researchers are working on a range of studies to improve the device and ready it for human trials. They hope to test their device on people in three years’ time.
The study is published in Nature Communications,