HQ Team
November 21, 2021: In type 2 diabetes the body loses the ability to release insulin, the hormone known to lower blood glucose levels. This is because a glucose metabolite damages pancreatic beta-cell function.
Now researchers at Oxford led by Dr Elizabeth Haythorne and Professor Frances Ashcroft of the Department of Physiology, Anatomy and Genetics have discovered that glucose metabolites rather than glucose are responsible for the progression of type 2 diabetes (T2D).
Using both an animal model of diabetes and beta-cells cultured at high glucose, they showed, for the first time, that a damaged glucose metabolism prevents beta-cells to release insulin in T2D. The research team also found that beta-cell failure caused by chronic hyperglycaemia can be prevented by slowing the rate of glucose metabolism.
Professor Ashcroft said: ‘This suggests a potential way in which the decline in beta-cell function in T2D might be slowed or prevented.’
Slowing decline in beta-cell function
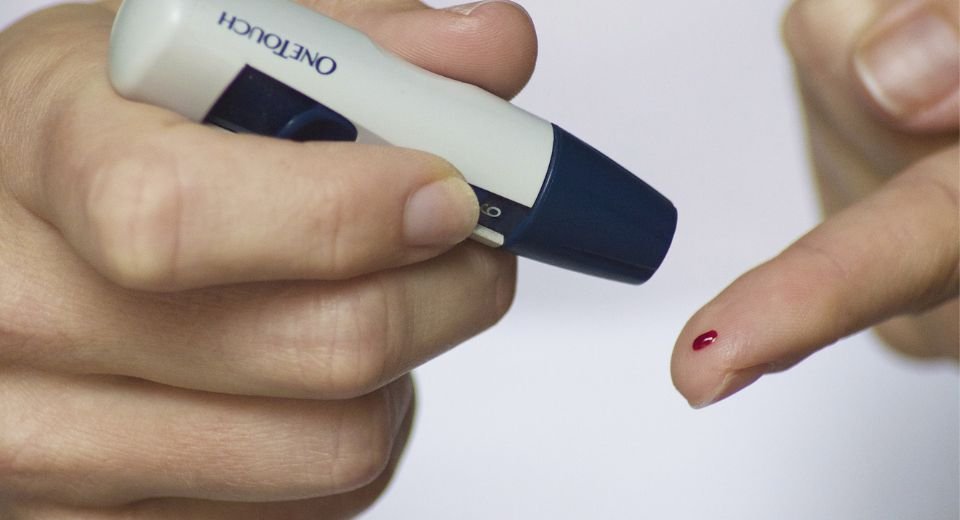
In the body, the blood glucose level needs to be controlled within a narrow limit. Too low levels can quickly lead to loss of consciousness. Chronic elevation of the blood gives rise to serious complications such as retinopathy, nephropathy, peripheral neuropathy, and cardiac disease. Insulin, released from pancreatic beta-cells when blood glucose levels rise, is the only hormone that can lower blood glucose concentration. In T2D, the beta-cells are still present (unlike T1D), but their functionality is reduced and they do not release the required amount of insulin.
Dr Haythorne said: ‘We realised that we next needed to understand how glucose damages beta-cell function, so we can think about how we might stop it and so slow the seemingly inexorable decline in beta-cell function in T2D.’
The present study shows that high blood glucose levels cause an increased rate of glucose metabolism in the beta-cell which leads to damaging metabolites. These metabolites switch off the insulin gene, as well as numerous genes involved in metabolism and stimulus-secretion coupling. Consequently, the beta-cells become glucose blind, that is they no longer respond to changes in the blood glucose levels.
The team found that blocking an enzyme called glucokinase, which regulates the first step in glucose metabolism, could prevent the gene changes taking place and maintain glucose-stimulated insulin secretion even in the presence of chronic hyperglycaemia.
Professor Ashcroft said: ‘This is potentially a useful way to try to prevent beta-cell decline in diabetes. Because glucose metabolism normally stimulates insulin secretion, it was previously hypothesised that increasing glucose metabolism would enhance insulin secretion in T2D and glucokinase activators were trialled, with varying results.
‘Our data suggests that glucokinase activators could have an adverse effect and, somewhat counter-intuitively, that a glucokinase inhibitor might be a better strategy to treat T2D. Of course, it would be important to reduce glucose flux in T2D to that found in people without diabetes – and no further. But there is a very long way to go before we can tell if this approach would be useful for treating beta-cell decline in T2D. In the meantime, the key message from our study, if you have type 2 diabetes, is that it is important to keep your blood glucose well controlled.’
An estimated 415 million people globally are living with diabetes. More than 95% of people with diabetes have type 2 diabetes. In 2019, diabetes and kidney disease due to diabetes caused an estimated 2 million deaths.
T2D normally presents in later adult life, and by the time of diagnosis, as much as 50% of beta cell function has been lost.
The full paper, ‘Altered glycolysis triggers impaired mitochondrial metabolism and mTORC1 activation in diabetic β-cells’, can be read in Nature Communications