HQ Team
September 5, 2024: Harvard Medical School scientists have designed an artificial intelligence model similar to ChatGPT that detects cancer or predicts a tumour’s genetic profile.
The AI model was tested on 19 cancer types and it may be the first to predict patient outcomes and validate them across several international patient groups, according to a Harvard statement.
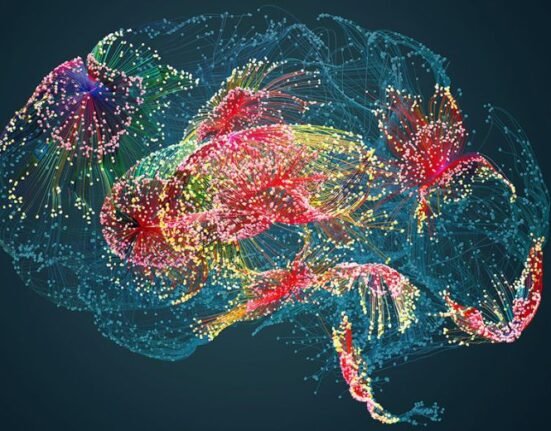
The AI model, which works by reading digital slides of tumour tissues, detects cancer cells and predicts a tumour’s molecular profile based on cellular features seen on the image with superior accuracy to most current AI systems.
“Our ambition was to create a nimble, versatile ChatGPT-like AI platform that can perform a broad range of cancer evaluation tasks,” said study senior author Kun-Hsing Yu, assistant professor of biomedical informatics at the Blavatnik Institute at Harvard Medical School.
“Our model turned out to be very useful across multiple tasks related to cancer detection, prognosis, and treatment response across multiple cancers.”
94% cancer detection accuracy
The model named CHIEF (Clinical Histopathology Imaging Evaluation Foundation), achieved 94% accuracy in cancer detection and significantly outperformed current AI approaches across 15 datasets containing 11 cancer types.
In five biopsy datasets collected from independent cohorts, the model achieved 96% accuracy across multiple cancer types including oesophagus, stomach, colon, and prostate.
When the researchers tested CHIEF on previously unseen slides from surgically removed tumours of the colon, lung, breast, endometrium, and cervix, the model performed with more than 90% accuracy.
It can forecast patient survival across multiple cancer types and accurately pinpoint features in the tissue that surrounds a tumour — also known as the tumour microenvironment — that are related to a patient’s response to standard treatments, including surgery, chemotherapy, radiation, and immunotherapy.
Model trained on 15 million images
CHIEF was trained on 15 million unlabeled images chunked into sections of interest.
The tool was then trained further on 60,000 whole-slide images of tissues including lung, breast, prostate, colorectal, stomach, oesophagal, kidney, brain, liver, thyroid, pancreatic, cervical, uterine, ovarian, testicular, skin, soft tissue, adrenal gland, and bladder.
The team tested the model’s performance on more than 19,400 whole-slide images from 32 independent datasets collected from 24 hospitals and patient cohorts across the globe.
“The model appears capable of generating novel insights — it identified specific tumour characteristics previously not known to be linked to patient survival,” according to the statement.
Overall, the new model outperformed other state-of-the-art AI methods by up to 36% on cancer cell detection, tumour origin identification, predicting patient outcomes, and identifying the presence of genes and DNA patterns related to treatment response.
DNA sequencing
The results add to the growing evidence that AI-powered approaches can enhance clinicians’ ability to evaluate cancers efficiently and accurately, including the identification of patients who might not respond well to standard cancer therapies.
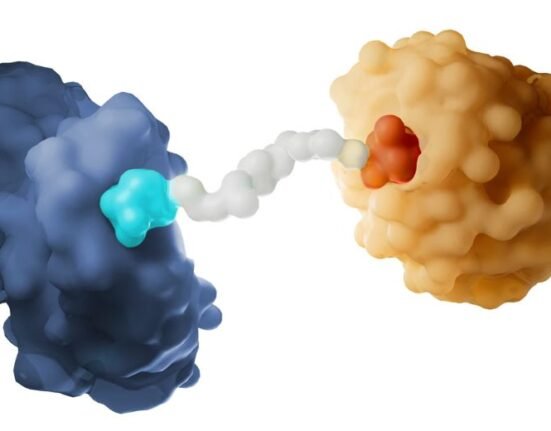
A tumour’s genetic makeup holds critical clues to determine its future behaviour and optimal treatments. To get this information, oncologists order DNA sequencing of tumour samples.
Detailed genomic profiling of cancer tissues is not done routinely nor uniformly across the world due to the cost and time involved in sending samples to specialized DNA sequencing labs.
Quickly identifying cellular patterns on an image suggestive of specific genomic aberrations could offer a quick and cost-effective alternative to genomic sequencing, the researchers said.