HQ Team
February 29, 2024: A long-term study of more than a thousand 70 years old people found that those exposed to the herpes simplex virus type 1 (HSV-1) were at greater risk of Alzheimer’s disease regardless of whether they had other markers such as genetic variants and cognitive impairment.
The study was carried out by researchers at Uppsala University and Umeå University in Sweden.
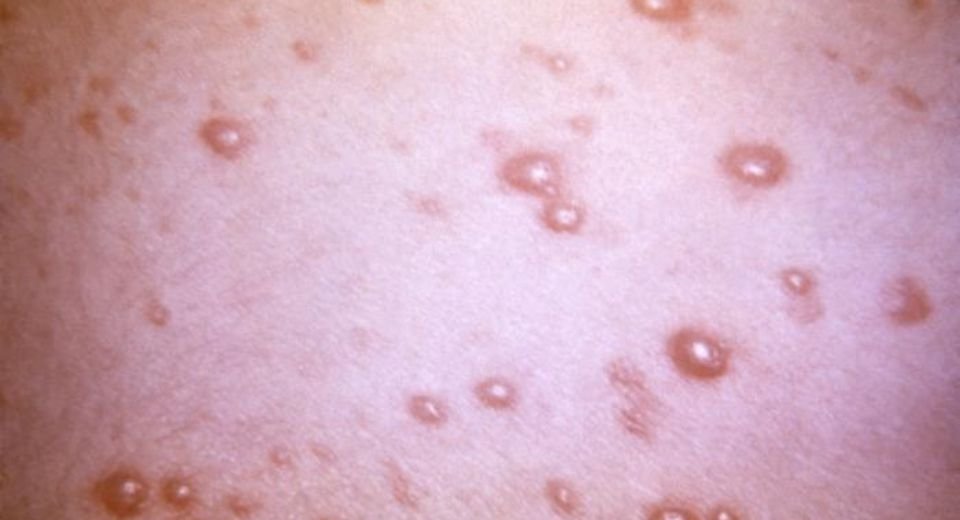
Experts say that studies have found that over 90 percent of the world population has the varicella-zoster virus lying dormant carried over from childhood. The same virus can become active in a third of these people as shingles also called herpes zoster. The annual incidence of the disease is estimated between 1.5 and 3.9 cases per 1,000 persons. About one million cases of shingles are diagnosed every year in the US with more than 50% reported in people above 50 years of age.
Today, roughly 80 percent of adults in Sweden carry the antibody for HSV-1, meaning their immune systems have been exposed to the pathogen at some point in the past.
Of the 1,002 adult participants that the researchers followed for 15 years, 82 percent were carriers of HSV-1 antibodies. These patients were twice as likely to develop dementia over the course of the study compared to those who did not carry HSV-1 antibodies. The new results from Sweden suggest HSV-1 could be having insidious effects on the inside. Interestingly, those participants who carried the genetic risk factor, APOE-4, were no more likely to show cognitive decline linked to HSV-1 antibodies.
“It is exciting that the results confirm previous studies,” says epidemiologist Erika Vestin from Uppsala University in Sweden.
“More and more evidence is emerging from studies that, like our findings, point to the herpes simplex virus as a risk factor for dementia.”
Abnormal protein clumps in Alzheimer’s
Alzheimer’s is the most common type of dementia, and it is oftentimes, but not always, marked by abnormal protein clumps in the brain.
Some experts now think they could play a role in the immune response of the central nervous system, repairing damage or preventing pathogens from causing damage. They now believe that Alzheimer’s could develop in some as an ‘out-of-control’ defense response to foreign microbes.
Previous studies
Infections as a cause of triggering Alzheimer’s disease were not new and were first proposed way back in 1907, but were faced with disregard. Only very recently has it been accepted as a probable cause.
Studies in the 90s of Alzheimer patients linked immune response to infections as a cause of dementia. In 2008, researchers discovered HSV-1 DNA was present in 90 percent of the protein plaques in postmortem brains of Alzheimer’s patients. What’s more, 72 percent of HSV-1 DNA in the brain was found within these plaques.
A recent meta-analysis of 500,000 medical records found that some severe viral infections, like encephalitis and pneumonia, may increase the risk of neurodegenerative diseases, such as Parkinson’s or Alzheimer’s.
However, no conclusive results have been endorsed to find a correlation between HSV-1 and dementia risk.
“What’s special about this particular study is that the participants are roughly the same age, which makes the results even more reliable since age differences, which are otherwise linked to the development of dementia, cannot confuse the results,” says Vestin.
The Swedish researchers want further research done to investigate whether herpes treatment could help prevent or stall the onset of dementia. There is an ongoing phase II clinical trial studying the effect of a herpes treatment on Alzheimer’s.
Such results “may drive dementia research further towards treating the illness at an early stage using common anti-herpes virus drugs, or preventing the disease before it occurs,” hopes Vestin.
The study was published in the Journal of Alzheimer’s Disease.