HQ Team
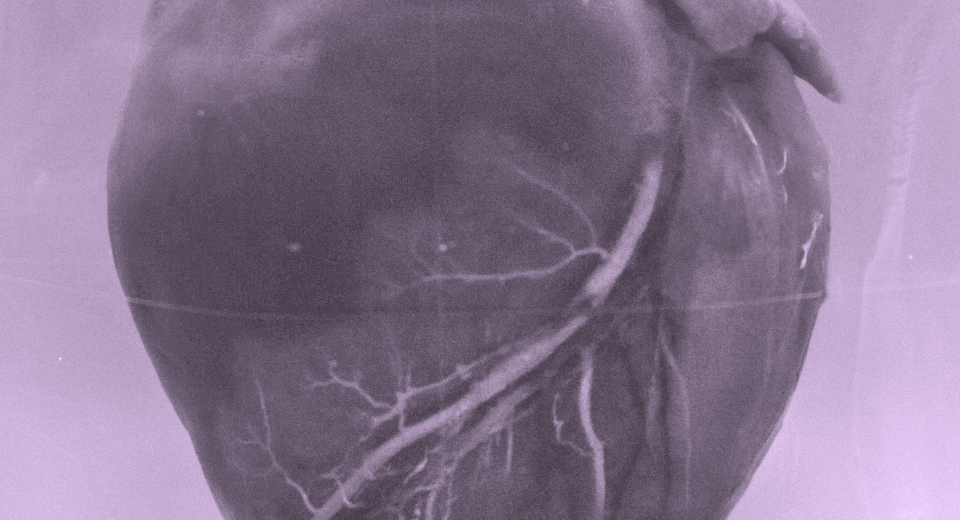
August 6, 2024: A new cardiovascular disease risk calculator may render 16 million US citizens ineligible for preventive therapy if the current guidelines for cholesterol and high blood pressure treatment remain the same, according to a Harvard Medical School study.
The risk calculator backed by American Heart Association, named as Presdicting Risk of Cardiovascular Events (PREVENT), is better calibrated and more precise than its previous version in 2013.
If the existing treatment “guidelines remain unchanged, the new calculator may have unintended consequences,” according to the study.
The Harvard Medical School study estimated that the risk calculator would render nearly 16 million people newly ineligible under current treatment thresholds that guide clinical decisions about who should get cholesterol and blood pressure drugs.
The change in treatment eligibility would be most pronounced among men between the ages of 50 and 69. The resulting decrease in access to statin and blood pressure therapy could lead to 107,000 additional heart attacks and strokes over the next 10 years, the analysis forecasted.
Recommended care
“The takeaway from our study is that updating risk estimation without reconsidering treatment thresholds has the potential to change recommended care for millions of Americans,” said study first author James Diao, a resident physician at Brigham and Women’s Hospital.
On the filip side it may reduce diabetic cases by about 57,000 over the same period, according to a statement from the medical school.
The new tool includes broader measures of health and provides sex-specific results but leaves out considerations of race, the American Heart Association stated.
It evaluates the risk of heart attack, stroke and – for the first time in such a calculator – heart failure. It also factors in new measures of cardiovascular disease, kidney disease and metabolic disease, which includes Type 2 diabetes and obesity.
Compared with the existing calculator, the new version allows health professionals to evaluate younger people and look further into the future.
Six million US adults
The new equations were developed using data from more than six million US adults from a variety of racial and ethnic, socioeconomic and geographic backgrounds.
A risk calculator allows a health care professional to use health data, such as blood pressure and cholesterol levels, as well as demographic and socioeconomic information to produce a risk estimate or score.
The risk calculator incorporates cardiovascular-kidney-metabolic syndrome, which was first defined by the AHA in October, 2023. It can assess people from ages 30 to 79 and can predict risk for heart attack, stroke and heart failure over the next 10 years and 30 years.
The previous calculator was designed for people starting at age 40 and looked only 10 years ahead.
The researchers based their projections on nearly 7,700 participants aged between 30 and 79 drawn from the US National Health Examination and Nutrition Survey and applied the 2013 and 2023 risk calculators to gauge risk and outcomes under each tool.
Statin, antihypertension
Based on this analysis, the researchers forecasted that the new risk calculator would reclassify nearly half of US population into lower risk categories. Very few people (less than 0.5 percent of the population) would be reclassified into higher risk categories under the new calculator.
The researchers then analyzed eligibility for statin and antihypertension treatment using current criteria, which call for treatment of most patients with intermediate and high risk and for a focused conversation for patients with borderline risk.
Under this new risk classification and the current treatment criteria, more than 14 million people would no longer qualify for cholesterol-lowering statins and 2.6 million would no longer qualify for medicines that control high blood pressure.
Removal of race
The removal of race from the recalibrated calculator would assign lower risk to more Black Americans and render more of them ineligible for therapy, compared with the previous version of the calculator, which did include race as a risk magnifier.
“But the analysis did not project a disproportionate rise in heart attacks and strokes in newly ineligible Black Americans, compared with White Americans. This surprising finding likely stems from preexisting disparities in access to preventive cardiovascular care,” the researchers wrote in the JAMA journal.
“We thought that if Black individuals became disproportionately less eligible for statins, they would be projected to have disproportionately more heart attacks and strokes, but our data did not reflect this expectation,” Diao said.
“We think this may be because fewer Black Americans have access to these medications and to recommended care to begin with. That’s a clear case of two wrongs don’t make a right.”