Bharti Jayshankar
January 26, 2024: A recent UK-based BRIGhTMIND trial sheds light on the comparable effectiveness and safety of two advanced neuromodulation MRI therapies in treating Treatment-Resistant Depression (TRD).
The study, encompassing 685 participants, showed sustained improvements in depression symptoms up to 26 weeks, opening new possibilities for individuals unresponsive to conventional treatments.
Personalized neuromodulation
The BRIGhTMIND trial explored advanced neuromodulation therapies, viz rTMS (repetitive transcranial magnetic stimulation) and cgiTBS (connectivity-guided intermittent theta burst stimulation) for Treatment-Resistant Depression (TRD), revealing significant insights into their effectiveness and potential for sustained response.
While repetitive TMS received FDA approval in the US in 2008, its implementation varies globally. Patchy adoption, especially in routine mental health practices outside North America, highlights the need for stronger evidence supporting its efficacy.
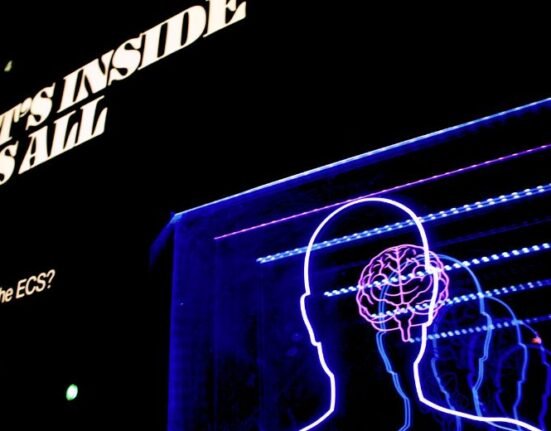
Transcranial Magnetic Simulation (TMS)
TMS is an outpatient treatment where people have powerful magnetic pulses delivered to the left side of their head just in front of the temporal area of the scalp. The person is conscious and has 20 sessions over a four-to-six-week period. The method has been used since the 1980s to treat people with severe depression, but by targeting the precise area of the brain where stimulation is thought to be helpful, researchers now have evidence for a longer-lasting benefit of this treatment.
The study emphasizes the importance of a personalized approach to neuromodulation, citing two small RCTs indicating greater responses in depression for personalized treatments. Individualizing the stimulation site based on functional connectivity leads to improved outcomes compared to standardized approaches.
BRIGhTMIND trial results
The multicenter BRIGhTMIND trial, conducted in the UK, involved 255 participants, examining the efficacy of cgiTBS and MRI-neuronavigated rTMS over 26 weeks.
Patients already in specialist mental health services were recruited, and both Primary Care trusts and GPs were approached, with all participants having to be referred by their GP to take part.
Encouraging response rates
Both treatment arms demonstrated clinically substantial improvements in depression symptoms. Around one-third of participants showed a response, one-fifth achieved remission and one-fifth experienced sustained response for six months.
Contrary to previous beliefs that the benefits of rTMS are short-lived, the trial’s results suggest sustained responses for more than six months post-treatment.
Major depression is the leading cause of disability lost years worldwide (WHO, 2017), and suicide from depression is the biggest killer in people aged between 15-49. Antidepressants and therapy delivered as first or second-line treatments help two-thirds of people with depression, but the remaining third have treatment-resistant depression (TRD).
The study delves into the mechanistic aspects of neuromodulation, suggesting a potential normalizing effect on brain dysconnectivity. The findings open doors to further research, indicating the possibility of keeping some TRD patients well and providing significant benefits for others through personalized neuromodulation.
The BRIGhTMIND trial offers a ray of hope for individuals struggling with Treatment-Resistant Depression, paving the way for more personalized and sustained treatment approaches. The study’s insights are expected to reshape the landscape of neuromodulation therapies, offering new possibilities for mental health care globally.
The results of the trial are published in Nature Medicine,