By K. Leelamoni
January 16, 2024: Vaccination is a simple, safe and effective method of protecting the body against infectious diseases.
Ever since Edward Jenner’s discovery of smallpox vaccine in 1976 and Louis Pasteur’s success story of preventing rabies through vaccination, vaccines emerged as an effective tool to prevent many infectious diseases.
All these vaccines were against pathogens like bacteria and viruses. However, developing vaccines against parasitic diseases like malaria remained a hurdle for scientists all over the world.
Though malaria vaccines have been in development since the 1960s, substantial progress has been made only in the last decade resulting in the release of the first vaccine RTS, S/ASO1 in 2021 and R 21 Matrix M in 2023.
Both vaccines were safe and effective against the deadly plasmodium falciparum malaria and were approved by the WHO.
Two instead of one
“As a malaria researcher, I used to dream of the day we would have a safe and effective vaccine against malaria. Now we have two, “said Dr. Tedros Adhanom Ghebreyesus, Director General, WHO. There were an estimated 247 million malaria cases and 619000 deaths globally in 2021.
The African region continues to shoulder the heaviest malaria load, comprising 95% of cases and 96% of deaths globally. Children are more vulnerable – nearly half a million African children die from malaria every year.
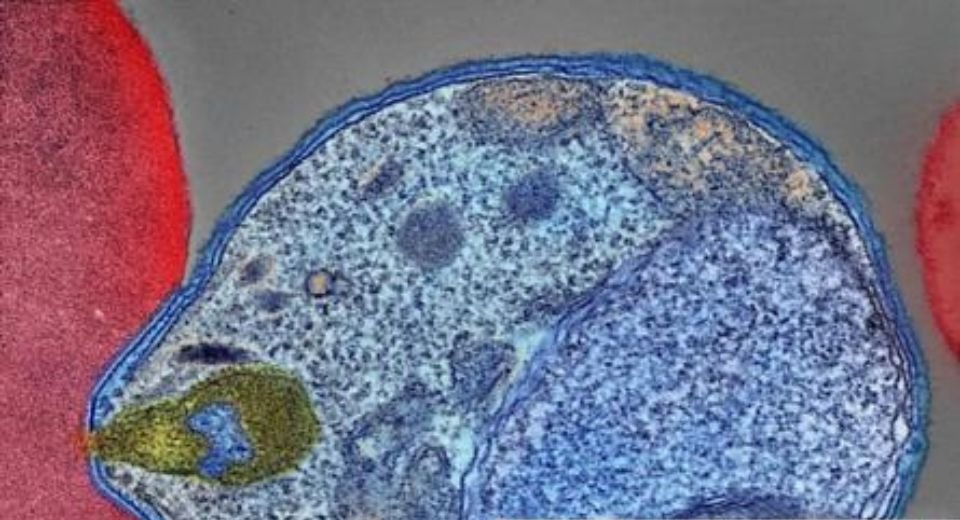
Malaria is a disease transmitted to man by the bite of the female Anopheles mosquito. It is caused by the parasite Plasmodium. There are five species of plasmodium of which plasmodium falciparum is the deadliest and poses the greatest threat in Africa.
Plasmodium vivax is the major parasite outside African countries. Malaria in children and pregnant women is dangerous. In pregnancy, it can result in premature delivery and low birth weight babies. Falciparum malaria can produce severe complications like severe anaemia, hypoglycemia, acute renal failure and hepatic impairment and can be life-threatening.
Why the delay?
Why was there a delay in the development of the malaria vaccine?
Compared to bacterial and viral vaccines, the development of a vaccine against the malarial parasite resulted in great frustration among scientists. Most important factor is the unique characteristics of the parasite, plasmodium.
It has a complex biology and genome and completes its life cycle in two hosts- man and mosquito. Moreover, it has an immune escape mechanism to evade the human immune system. To overcome these obstacles, research continued using components of different stages of the parasite during its life cycle. Efforts were concentrated on the sporozoites which are the infective form of the parasite in the saliva of the mosquito which enters the human body through mosquito bite.
The Circum Sporozoite Protein (CSP) is a major antigen component on the surface of the malaria sporozoites and it has been the main focus in vaccine development.
Malaria Vaccines:
1) RTS, S vaccine
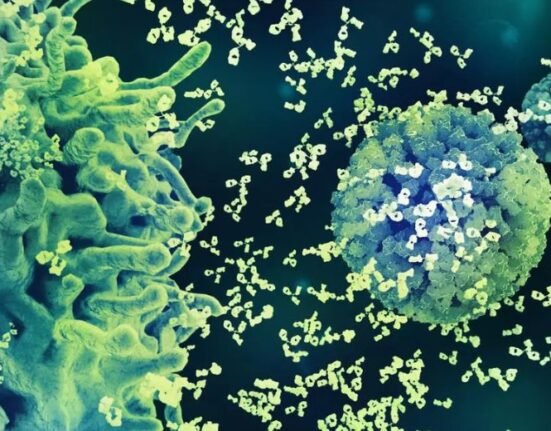
It was a historic day when the WHO approved the first malaria vaccine RTS, S also known as Mosquirix on October 6, 2021. It was developed by the PATH Malaria Vaccine Initiative and GlaxoSmithKline (GSK). It is a recombinant vaccine consisting of the falciparum CSP. Vaccination with RTS, S induces antibodies against CSP and immobilises the sporozoites thereby preventing infection of the liver cells (hepatocytes).
2) R 21 Matrix /M vaccine
This is an improved version of RTS, S developed by the Jenner Institute in Oxford, UK and the Serum Institute of India.
This vaccine also bears a CSP antigen and the adjuvant used is Matrix M. This has a higher efficacy level of 77% and the antibody level is significantly higher than RTS, S. Both vaccines are safe and effective against the deadly falciparum malaria and when given showed substantial impact in reducing paediatric hospitalisation for severe malaria and saving lives.
Schedule of vaccination:
The vaccine is recommended to be given in a schedule of 4 doses (intramuscular) in children from 5 months of age. The 4th dose given after one year of the 3rd dose, helps to maintain the efficacy. In areas of high risk, a 5th dose may be considered a year after the 4th dose.
Side effects:
Known side effects include pain and swelling at the injection site and fever which are similar to other vaccines are given to children.
Twenty-eight countries in Africa plan to introduce the malaria vaccine as part of their National Immunization program. The RTS, S vaccine will be rolled out first in some countries by early 2024 and the R21 Matrix M by mid-2024.
Constraints in vaccine production
-Lack of a traditional market
-Few developers for the vaccine
-Technical complexity of developing a vaccine against a parasite
-Financial considerations
-Lack of a robust health care infrastructure in malarial endemic countries
However, about 60 years of malaria research has resulted in the development of highly effective vaccines against the human malaria parasite Plasmodium falciparum. This was made possible only by the highly challenging recent innovations in malaria research.
The evolution of Public Private Partnerships such as the Malaria Vaccine Initiative of the Bill and Melinda Gates Foundation also offered hope for malaria research.
In India also, although remarkable progress has been made in the reduction of malaria incidence in recent years, a new vaccine against the deadly falciparum malaria can give this trend a boost. The vaccine will escalate India’s plans to be a malaria-free country in 2027 and complete elimination by 2030.
(The writer was a former Head of the Department of Community Medicine at the Government Medical College in Kozhikode and Thiruvananthapuram and worked at the Amrita Institute of Medical Sciences in Kochi.)





2 Comments