HQ Team
September 28, 2023: US scientists have honed in on a single chimeric antigen receptor T-cell (CAR T) therapy to cure all forms of blood cancer.
A research team at the University of Pennsylvania Perelman School of Medicine performed experiments in mice and found the therapy destroyed tumours, even in mammals with acute myeloid leukaemia.
Chimeric antigen receptor T-cell therapy gets immune cells or T-cells in white blood cells, to combat cancer by changing them in the lab so they can search and destroy cancer cells.
“There was also no evidence of serious side effects in the animals,” according to a statement from the National Institutes of Health’s National Cancer Institute.
“And finally, — and distinctly from the standard approach to current CAR T-cell therapies—it provided the mice with a healthy supply of new blood cells.”
CRISPR technology
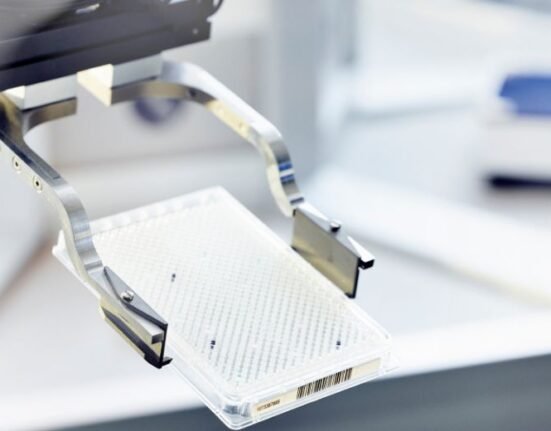
The therapy relies on CRISPR (clustered regularly interspaced short palindromic repeats) technology that research scientists use to selectively modify the DNA of living organisms.
CRISPR was adapted for use in the laboratory from naturally occurring genome editing systems found in bacteria, according to the National Human Genome Research Institute.
“In a unique twist for CAR T-cell therapy, it’s not only T cells that undergo genetic engineering. The treatment also involves engineering healthy hematopoietic stem cells,” according to the NIH statement.
The stem cells are the “immature” cells that generate all the body’s blood cells, including immune cells (like T cells), and form the basis for the stem cell transplants commonly used to treat blood cancers.
Cloak of invisibility
In the new treatment approach, the CRISPR editing resulted in a slight change to a protein, called CD45, that sits on the surface of both the CAR T cells and the stem cells.
This impostor CD45 protein provides noncancerous cells with a cloak of invisibility.
In lab experiments, the epitope-edited CD45-targeted CAR T cells worked as intended, killing several different types of blood cancer cells, but not killing each other or what is called “fratricide”.
In mice, the treatment shrank tumours and, as in the lab experiments, the T cells did not turn on each other.
Dr Saar Gill, one of the study’s lead investigators, and his colleagues first identified the epitopes on the CD45 protein where different CARs they had developed could bind.
Clinical trials
The end result was a CAR T-cell therapy that could kill any type of blood cancer cell — and only blood cancer cells — while giving patients a healthy blood and immune system.
It eliminates the need to go through the laborious and time-consuming process of developing and testing single therapies for specific blood cancers.
“We’re very determined to get this into a clinical trial,” said Dr Gill, from Penn’s Abramson Cancer Center, who along with his colleagues identified the epitopes of CD45 protein.
“It’s the only way we’ll know if it’s going to work. We think it’s doable within 2 years,” Dr Gill said.
Details of how it will pan out are sketchy he said.
Beam Therapeutics
“For example, whether the T cells and stem cells to be edited will be collected from patients themselves, or instead, if they will come from healthy donors.”
The study was published in Science Translational Medicine.
Researchers from other companies and universities are also working on CAR T cell therapies.
In early September, Beam Therapeutics announced that the first patient had been treated in a clinical trial of the company’s base-edited CAR T-cell therapy.
The Penn research team, led by Carl June, is already working on advancing their universal treatment approach to clinical trials.