By K. Leelamoni
January 30, 2024: Globally, we find that for the last few decades, there has been a shift towards non-communicable diseases (NCDs), due to the rising incomes leading to unhealthy lifestyles.
These diseases account for about more than 80% of the disease burden.
Most NCDs like cancer, cardiovascular diseases, dementia and chronic obstructive pulmonary disease result in long-term illnesses that need palliative care.
Increased life expectancy also leads to more chances of prolonged suffering from these chronic diseases. As per the World Bank data 2020, the life expectancy is about 77.28 years in the US, 70.15 years in India and 84.62 years in Japan.
In Kerala, it is 75.9 years. The ageing population and rise in the burden of NCDs point to the need for palliative care services.
Growing discipline
Palliative care has emerged as a growing discipline. It improves the quality of life of patients and that of their families who are facing challenges associated with life-threatening illness, whether physical, psychological, social or spiritual.
Palliative care is needed in a wide variety of diseases, mostly in CVDs (38.5%), cancer (34%) and chronic respiratory disease(10.3%).
Others include chronic liver disease, rheumatoid arthritis, Parkinsonism, dementia other neurological diseases and kidney failure.The quality of life of the caregivers also has improved.
I am reminded of the experience of a close relative of mine who was suffering from dementia.
A doctor himself, Gopal was a very jovial person and affectionate. When his daughter from the US came to see him he talked with her pleasantly and said: “My daughter is also in the US.”
His wife and daughter were shocked to hear this. His wife was depressed. However, the timely intervention by the local palliative care team helped her a lot to understand his condition and cope with it.
56.8 million a year
More than the patient, the close family members get benefit from palliative care.
Each year, an estimated 56.8 million people need palliative care.
Of these only 14% of people currently receive it.
Since palliative care involves a range of services, the palliative care team consist of physicians, nurses, pharmacists, physiotherapists, support workers and volunteers. Each of them has an important role to play in support of the patient and their families.
The treatment plan under palliative care includes pain control, nutrition, emotional and spiritual well-being, and accessibility.
Pain control
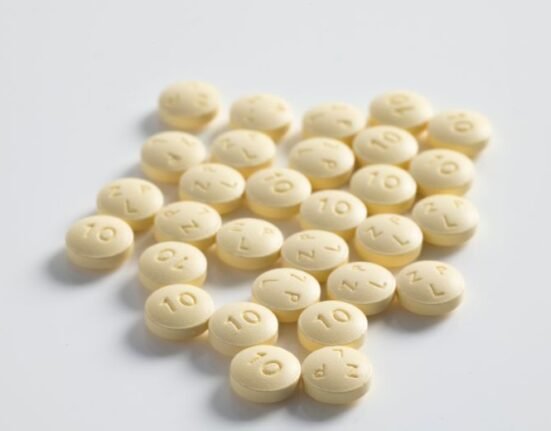
Pain and difficulty in breathing are two of the most common and serious symptoms experienced by patients who need palliative care.
A palliative pain relief program starts with drugs like ibuprofen and acetaminophen or with stronger medicines such as opioids. Sometimes opioids become essential for pain management.
They can also alleviate other common distressing symptoms including breathlessness. Controlling such symptoms at an early stage is an ethical duty to relieve suffering and to respect a person’s dignity.
Nutrition
Considering the dietary needs, ability to eat and digest and based on personal and cultural preferences, a diet plan can be charted out.
Emotional and spiritual wellbeing
Patients and their families may feel exhausted, anxious or lonely. This can result in fear, anger, confusion, grief and sadness that can add to the physical suffering.
Combating these difficult emotions is easier with support from the palliative care team.
Palliative care centres provide holistic care and support to critically ill patients by providing personalised care and treatment plans to improve the quality of life and reduce suffering. Patients may receive palliative care in a hospital, an outpatient clinic or at home.
Home-based palliative care services take services to the doorstep of the people. This is where people are more comfortable among their family members.
In the cases of long and potentially life-threatening illness, it provides care and backup support needed to prepare to face the days ahead.
Palliative care is most effective when considered early in the course of an illness. Early palliative care not only improves the quality of life of patients but also reduces unnecessary hospitalisation.
Accessibility
Though the need for palliative care is increasing, its acceptance and accessibility are limited to a great extent.
Lack of awareness among the health professionals and the public is a major factor. Misconceptions like palliative care is needed only for cancer and for the terminally ill and wrong concepts about opioid analgesia are other factors.
There is also a dearth of trained medical and paramedical professionals in palliative care.
Pallium India
In this context, the work done by Pallium India is praiseworthy. It is a nationally registered charitable non-governmental trust whose founder chairman is Padma Shri Dr. M. R. Rajagopal.
It works with national and international organisations to improve the accessibility and affordability of pain relief drugs (opioids) and other low-cost medicines and to improve the quality of palliative care services provided by the health and allied health professionals.
Pallium India works with several hospitals and organisations to develop palliative care centres and to provide palliative care education to professionals. In April 2022, they have started a free Telehealth consultation for patients and families anywhere in India.
Palliative care needs to be provided as an integral part of the health care system of the country. All people irrespective of income, disease type or age should have access to palliative care.
A sustainable and accessible palliative care system of good quality is a need of the day and every health professional should consider it as an ethical duty also.
(The writer was a former Head of the Department of Community Medicine at the Government Medical College in Kozhikode and Thiruvananthapuram and worked at the Amrita Institute of Medical Sciences in Kochi.)







1 Comment