HQ Team
December 13, 2022: A new meta-study has found that some supplements help lower the risk of heart disease better than others.
Researchers from Brown University gathered data from 884 studies with over 883.000 patients to review the effect of micronutrients taken as supplements. They reviewed 27 different types of dietary supplements and identified the ones that reduced the risk of heart problems such as attacks, strokes and those that had a negative impact on heart health.
Using data from 884 studies and more than 883,000 patients, researchers at Brown University systematically reviewed all of the existing evidence on micronutrients taken as dietary supplements. After evaluating 27 different types, they identified several that reduced the risk of cardiovascular problems like heart attack or stroke and others that offered no benefit or even had a negative effect.
The study’s lead investigator, Simin Liu, MD, MPH and professor of epidemiology and medicine at Brown University, said in a press release. “Our study highlights the importance of micronutrient diversity and the balance of health benefits and risks.” He added that it was one of the first comprehensive studies done on the impact of supplements on heart health.
The research found the strongest evidence of heart benefits could be found in Omega-3 fatty acids or fish oil, Folic acid, and Coenzyme Q10.
Other supplements showing evidence of reducing cardiovascular risk were omega-6 fatty acid, L-arginine, L-citrulline, vitamin D, magnesium, zinc, alpha-lipoic acid, melatonin, catechin, curcumin, flavanol, genistein, and quercetin.
Potentially harmful supplements for heart health
The research found that some supplements had no benefits or even could be harmful to cardio health. Vitamin C, vitamin E, and selenium showed no effect on long-term cardiovascular disease outcomes.
One concerning finding was that beta-carotene supplements which convert to vitamin A in our bodies, could potentially increase all-cause mortality. The findings are in line with the US Preventive Services Task Force’s (USPSTF) guidance not to take vitamin A supplements without consulting a doctor due to the risk of toxicity, which can lead to muscle and bone pain, nausea, and hair loss.
The study authors called for large, high-quality interventional trials to investigate the long-term effects of certain micronutrients.
Antioxidant supplements vs antioxidant-rich foods
Antioxidant supplements are seen as reducing “oxidative stress,” a known contributor to many types of cardiovascular disease. The Mediterranean diet and food that is naturally rich in antioxidants feature as dietary recommendations for better heart health..
But earlier research has shown some inconsistencies in the benefits provided by antioxidant supplements. Experts say the nutrients in supplements aren’t exactly the same as those in foods and hence are the reason why supplements haven’t been widely adopted in preventive cardiology, according to the authors.
“Previously, research on micronutrient supplementation has mainly focused on the health effects of a single vitamin or mineral or a few at a time, said Dr. Liu. “We decided to take a comprehensive and systematic approach to evaluate all the publicly available and accessible studies reporting all micronutrients, including phytochemicals and antioxidant supplements and their effects on cardiovascular risk factors as well as multiple cardiovascular diseases.”
Check with your doctor first if you need supplements
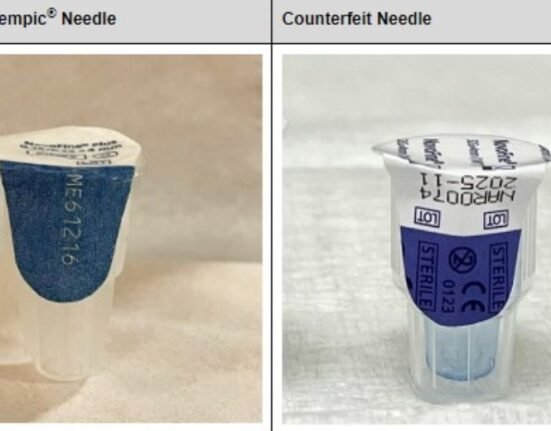
Beware that if doctors recommend a supplement, different brands can vary in quality. Ask specific questions about the dosage and ingredients and read the labels carefully.
The meta-analysis was published in the Journal of the American College of Cardiology.